Stroke:串联病变者,颅外颈动脉是否应该紧急支架置入?
2019-03-31 杨中华 脑血管病及重症文献导读
对于急性缺血性卒中,颅外颈动脉并串联颅内大动脉闭塞者预后不良。在不同血管内血栓切除术的随机试验中,串联病变的管理方法差异较大,有些把颅外颈动脉闭塞排除在试验以外,比如SWIFT PRIME 和 EXTEND IA 试验。在 MR CLEAN 试验(32.3%)、REVASCAT 试验(18.6%)和 ESCAPE 试验(17%)中,串联病变占的比例很高。尽管占比很高以及不治疗者预后
对于急性缺血性卒中,颅外颈动脉并串联颅内大动脉闭塞者预后不良。在不同血管内血栓切除术的随机试验中,串联病变的管理方法差异较大,有些把颅外颈动脉闭塞排除在试验以外,比如SWIFT PRIME 和 EXTEND IA 试验。在 MR CLEAN 试验(32.3%)、REVASCAT 试验(18.6%)和 ESCAPE 试验(17%)中,串联病变占的比例很高。尽管占比很高以及不治疗者预后很差,但是其最佳治疗策略仍然不清楚。
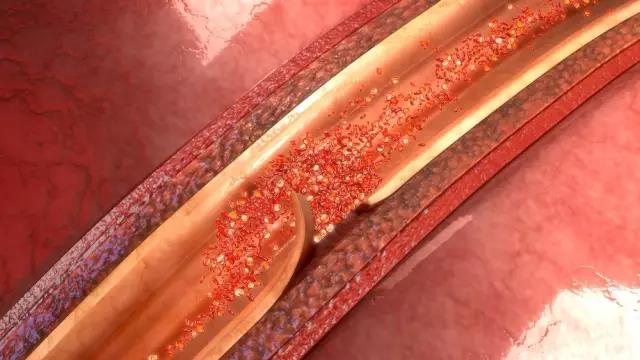
颅内闭塞者采取血管成形术是一种标准治疗策略,但是颅外病变的最佳管理策略差异很大并且缺乏一致性意见。单中心和多中心研究以及临床试验分析提示紧急置入支架是合理的;不过,仍然缺乏最佳管理的数据,因为置入支架通常需要立即双联抗血小板治疗,人们担心紧急置入支架后的安全性,因为有些研究发现脑出血的风险较高,另外也有作者建议出于安全性的考量应该延迟支架置入。
STRATIS 登记研究并未对串联病变的管理进行限制,因此允许研究者比较不同治疗策略的差异。2019年2月来自美国的Ashutosh P. Jadhav等利用 STRATIS 登记研究的数据,分析了在急性卒中血栓切除术中紧急置入颅外支架的临床和手术结局的差异,该研究发表在 Stroke 杂志上。
STRATIS 登记研究为前瞻性,非随机研究,纳入的患者(984例)采用 Solitaire 支架进行了血管内血栓切除术。其中147例(14.9%)为合并串联病变的患者,80例进行了颅外动脉支架置入,67例未置入支架。两组的年龄、ASPECTS 评分或静脉溶栓率没有差异。不过,支架置入组的基线 NIHSS 评分(16 vs 17.9;P = 0.07)更低,从发作到动脉穿刺时间(133.6 vs 163.4 min;P = 0.04)更短,合并房颤的比例更低(6.3% vs 25.4%)。与未置入支架相比,支架组的良好预后比例更高(90天 mRS 0-2)(68.5% vs 42.2%,P = 0.003),死亡率和症状性出血没有差异。调整协变量后,置入支架仍然与优良预后有关。
最终作者认为血管内血栓切除期间颅外颈动脉狭窄紧急置入支架与不置入支架安全性相当。急性期颈动脉置入支架预后更好;该结果需要被随机试验确认。
原始出处:Jadhav AP, Zaidat OO, Liebeskind DS, et al. Emergent Management of Tandem Lesions in Acute Ischemic Stroke. Stroke. 2019 Feb;50(2):428-433.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#颈动脉#
20
谢谢分享
60
谢谢分享
67
#紧急#
25
学习
67
学习
55
学习
66