痣少的患者可能意味着其黑色素瘤的侵袭性更高
2015-08-23 MedSci MedSci原创
痣少的患者可能意味着其黑色素瘤的侵袭性更高身上痣的数目多余50的个体患黑色素瘤的风险会增加,但是少于50个痣的个体也应警惕黑色素瘤的发生。据2015年美国皮肤学院夏季会议的一项最新研究显示,与痣多的人相比,痣少的人发生侵袭性更强的黑色素瘤的风险更大。Dr. Kim说道,对于身上痣多余50个的人来说,他们可能更清楚自己患癌的风险,更可能去皮肤科筛查,然而,在治疗晚期皮肤黑色素瘤病例时,她发现,身上痣
身上痣的数目多余50的个体患黑色素瘤的风险会增加,但是少于50个痣的个体也应警惕黑色素瘤的发生。据2015年美国皮肤学院夏季会议的一项最新研究显示,与痣多的人相比,痣少的人发生侵袭性更强的黑色素瘤的风险更大。
Dr. Kim说道,对于身上痣多余50个的人来说,他们可能更清楚自己患癌的风险,更可能去皮肤科筛查,然而,在治疗晚期皮肤黑色素瘤病例时,她发现,身上痣更少的患者其黑色素瘤的侵袭性更强。
为了探究痣多与痣少之间黑色素瘤的差别,Dr. Kim及其同事回顾分析了281例黑色素瘤患者。89名患者身上痣的数目多余50个,其余192名患者身上痣的数目低于50个。
结果发现,相对于痣多的患者,痣少的患者其黑色素瘤更厚、侵袭性更强;痣多且不典型的患者其黑色素瘤更薄且侵袭性更弱。此外,与痣多的患者相比,痣少的患者诊断出黑色素瘤的年龄更小。
Dr. Kim认为她们的研究结果可能是由几个因素所造成。卫生保健提供者可以很容易的确定痣多于50个的个体患癌的风险更大,并告知患者重视其患癌风险。其结果是,这些人更可能定期去接受皮肤检查,因而便可在黑色素瘤早期,较薄且侵袭性较弱的时候检测出来。
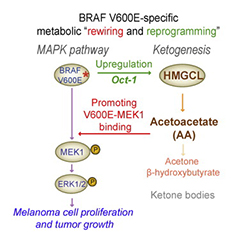
此外,痣多与痣少患者存在生物学上的差异,而且这些差异可能是导致黑色素瘤存在差异的原因。Dr. Kim说道,“我们已经知道,导致黑色素瘤发生的突变的基因并不完全相同。这两种患者发生黑色素瘤的途径很可能并不相同,导致了黑色素瘤侵袭性的不同。如果痣少的患者更易发生侵袭性更强的黑色素瘤,那么我们就需要确保他们也接受教育和筛查。”
Dr. Kim表示仍需要更大规模的研究以证实她们的研究成果。进一步探究这两组患者黑色素瘤的生物学特性将十分重要,研究人群皮肤癌筛查的益处意味着扩大皮肤癌检查工作的必要性。
“这项研究提醒我们,每个人都需要警惕黑色素瘤,不管他们身上痣多还是少,”Dr. Kim说道,“确保你知道如何识别皮肤癌发生时的迹象,且在怀疑患癌时及时就诊。”
原始出处:
Study: Fewer Moles May Mean More Aggressive Melanoma.Newswise,17-Aug-2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#色素#
21
#侵袭性#
22
#痣#
28
#黑色素#
19
#黑色素#
29