珍藏:四大医学期刊近期个案病例报道汇总(附总结评论)必看!
2015-11-06 Kelly MedSci原创
由于个体和疾病本身的不可预测性,病人可能会出现不寻常的症状,或对于医学干预出现以前没有见过的反应方式。发表这些新奇的发现是医学知识发展的根本途径。 Kaposi’s 肉瘤的年轻同性恋男子的病例报告发现了获得性免疫缺陷综合征; 1817年James Parkinson报道的标题为“震颤性麻痹”一文导致了帕金森氏病的发现; Shiga毒素大肠杆菌引起溶血性尿毒综合征;
由于个体和疾病本身的不可预测性,病人可能会出现不寻常的症状,或对于医学干预出现以前没有见过的反应方式。发表这些新奇的发现是医学知识发展的根本途径。
Kaposi’s 肉瘤的年轻同性恋男子的病例报告发现了获得性免疫缺陷综合征;
1817年James Parkinson报道的标题为“震颤性麻痹”一文导致了帕金森氏病的发现;
Shiga毒素大肠杆菌引起溶血性尿毒综合征;
1985年美国医学协会重新印刷了该协会存在150年以来美国医学协会杂志(JAMA)上发表的显著改变了医学科学51篇论文,这些论文中5篇是病例报告。
随着时间的推移,病例报告类论文目前已主要集中在已知疾病的特殊临床表现、影像学及检验学等诊断手段的新发现、疾病的特殊临床转归、临床诊断治疗过程中的特殊的经验和教训等。
我们先来看近期四大医学期刊发表的几篇个案病例报道。
案例一、BMJ:“大脚趾疼痛10年”
70岁老年女性右大脚趾疼痛10年。近节指骨骨节突出。X线提示皮质增厚,侵入骨髓腔;可见明显粗小梁;近节指骨骨质的扩张。




该患者诊断为:(大脚趾)单骨性 Paget's病。
讨论:
可能的诊断有:Paget's病、骨转移癌、感染性指炎、银屑病性关节病、肢骨纹状肥大。
基于临床表现和影像学资料诊断为单骨性 Paget's病。因为缺乏系统性症状,并且该表现长期存在,所以不大可能是感染性指炎、骨转移癌和银屑病性关节病。粗小梁可排除肢骨纹状肥大诊断。
随着年龄增长Paget's病越来越常见,男性多余女性。西方国家该疾病的患病率有明显的地区差异,有报道称20世纪70年代英国患病率最高。
疼痛可能是由于患骨发生微小骨折导致的;因为患骨变性的关节面,会导致相邻关节的骨关节病。
该患者的治疗包括使用鞋垫和非甾体抗炎药(缓解疼痛)。
原始出处:Lui TH, Tam KF,et al.An unusual case of a painful big toe.BMJ. 2015 Aug 25;351:h4533.
讨论:
可能的诊断有:Paget's病、骨转移癌、感染性指炎、银屑病性关节病、肢骨纹状肥大。
基于临床表现和影像学资料诊断为单骨性 Paget's病。因为缺乏系统性症状,并且该表现长期存在,所以不大可能是感染性指炎、骨转移癌和银屑病性关节病。粗小梁可排除肢骨纹状肥大诊断。
随着年龄增长Paget's病越来越常见,男性多余女性。西方国家该疾病的患病率有明显的地区差异,有报道称20世纪70年代英国患病率最高。
疼痛可能是由于患骨发生微小骨折导致的;因为患骨变性的关节面,会导致相邻关节的骨关节病。
该患者的治疗包括使用鞋垫和非甾体抗炎药(缓解疼痛)。
原始出处:Lui TH, Tam KF,et al.An unusual case of a painful big toe.BMJ. 2015 Aug 25;351:h4533.
案例二、NEJM:随地大小便,阴茎被蛇咬病例报道
内含高能图片,已关注粉丝可直接回复关键词查看(同在线和APP浏览),若尚未关注,可识别二维码一键关注后回复关键词“阴茎被蛇咬”查看详情。
案例三、NEJM:一例关于胃复安药物副作用的案例报道
女性,21岁,患有甲状腺癌,行甲状腺全切除术及淋巴结清扫术后。
术后第二天,该患者开始出现颈部后仰,下巴难以闭合,以及眼睛无节律性横向偏移(请观看视频1)。此外,她目前尚能听从指令进行活动(例如,她能按照要求伸出舌头)。

随后,主治医师对其停用胃复安药物。
据研究,类似于本案例中患者使用胃复安药物后所出现的副作用是非常罕见的,发病率通常只限于儿童和年龄小于30岁,或是每天使用剂量>30mg/天和使用频率太频繁才会导致。
因此,主治医师建议该患者日后用药一定要慎用胃复安此药物。
术后第二天,该患者开始出现颈部后仰,下巴难以闭合,以及眼睛无节律性横向偏移(请观看视频1)。此外,她目前尚能听从指令进行活动(例如,她能按照要求伸出舌头)。

据了解,该患者在术后为了抑制恶心症状曾遵医嘱服用过胃复安这个药物,10mg/次,每天2次,连续服用2天,在恶心症状开始发作的24小时后开始服用。服用后便开始出现以上的临床症状。
为了消除该患者颈部急性肌张力障碍症状,主治医师采用一种静脉注射药物比哌立登(抗胆碱能药物)进行治疗,几分钟后肌张力障碍症状开始消失(请观看视频2)。
为了消除该患者颈部急性肌张力障碍症状,主治医师采用一种静脉注射药物比哌立登(抗胆碱能药物)进行治疗,几分钟后肌张力障碍症状开始消失(请观看视频2)。
随后,主治医师对其停用胃复安药物。
据研究,类似于本案例中患者使用胃复安药物后所出现的副作用是非常罕见的,发病率通常只限于儿童和年龄小于30岁,或是每天使用剂量>30mg/天和使用频率太频繁才会导致。
因此,主治医师建议该患者日后用药一定要慎用胃复安此药物。
原始出处:Leus M, van de Ven A.IMAGES IN CLINICAL MEDICINE. An Acute Dystonic Reaction after Treatment with Metoclopramide. N Engl J Med. 2015
案例四、Lancet:骨折后致脑脂肪栓塞
44岁男性,因车祸导致右腓骨和胫骨、左股骨、骨盆等多处骨折。为稳定左股骨行PFNA(新型股骨近端内固定系统)。
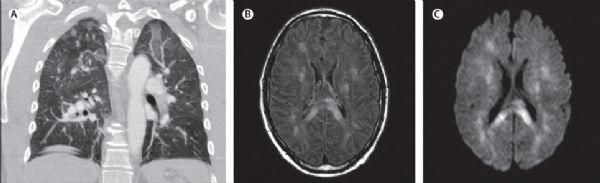
术后1小时,患者突发急性呼吸衰竭,立即行气管插管,转入ICU治疗。完善胸部CT血管造影:双侧肺毛玻璃改变;明显的结节状影;没有发现肺栓塞征象。
术后1小时,患者突发急性呼吸衰竭,立即行气管插管,转入ICU治疗。完善胸部CT血管造影:双侧肺毛玻璃改变;明显的结节状影;没有发现肺栓塞征象。
有创呼吸机辅助通气的情况下,患者低氧血症一直难以纠正(血氧分压6.7kPa,正常为11–13 kPa)。患者出现发热和心动过速,开始使用抗生素治疗。4天后,停止镇静药物的使用,并进行格拉斯哥昏迷评分(GCS)为3分。患者的腋窝和腹股沟区域开始出现瘀点,术后第10天行头颅MRI检查:双侧白质融合异常伴扩散受限。这种白质病变(而不是灰质)导致的细胞毒性脑水肿,提示亚急性脂肪栓塞(栓塞后5-14天)。
脑电图:弥散性脑病。
在急性呼吸衰竭的基础上,腋窝和腹股沟的出血表现,以及MRI上的典型征象,患者诊断为:脑型脂肪栓塞综合征。超声心动图没有发现卵圆孔未闭或从右到左的分流。
继续对患者进行支持性治疗,术后16天,患者呼吸和神经功能好转,予以拔除气管插管。最后患者转入神经康复中心继续治疗。
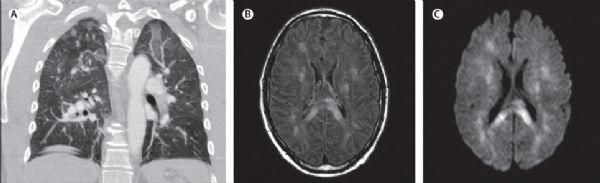
讨论:通常在骨髓移位造成的脑脂肪栓塞患者中观察到“呼吸衰竭+失去意识+瘀点”,常见于骨盆和长骨骨折,或使用髓内设备对骨折维稳时。创伤后骨髓脂肪可进入血液循环,导致肺栓塞。肺血流动力学改变和系统性炎症反应导致急性呼吸衰竭。柔软的脂肪栓子随后可以通过肺毛细血管到达皮肤、大脑等,导致皮肤瘀点和脑缺血神经症状。脑脂肪栓塞的诊断主要靠临床表现,MRI可以辅助该诊断:在急性期(1-4天)表现为散点病灶伴扩散限制;亚急性期(5-14天)表现为脑室周围和白质融合的细胞毒性脑水肿。
原始出处:Aman J, van Koppenhagen L,et al.Cerebral fat embolism after bone fractures.Lancet. 2015 Oct 3;386(10001):e16.
脑电图:弥散性脑病。
在急性呼吸衰竭的基础上,腋窝和腹股沟的出血表现,以及MRI上的典型征象,患者诊断为:脑型脂肪栓塞综合征。超声心动图没有发现卵圆孔未闭或从右到左的分流。
继续对患者进行支持性治疗,术后16天,患者呼吸和神经功能好转,予以拔除气管插管。最后患者转入神经康复中心继续治疗。
讨论:通常在骨髓移位造成的脑脂肪栓塞患者中观察到“呼吸衰竭+失去意识+瘀点”,常见于骨盆和长骨骨折,或使用髓内设备对骨折维稳时。创伤后骨髓脂肪可进入血液循环,导致肺栓塞。肺血流动力学改变和系统性炎症反应导致急性呼吸衰竭。柔软的脂肪栓子随后可以通过肺毛细血管到达皮肤、大脑等,导致皮肤瘀点和脑缺血神经症状。脑脂肪栓塞的诊断主要靠临床表现,MRI可以辅助该诊断:在急性期(1-4天)表现为散点病灶伴扩散限制;亚急性期(5-14天)表现为脑室周围和白质融合的细胞毒性脑水肿。
原始出处:Aman J, van Koppenhagen L,et al.Cerebral fat embolism after bone fractures.Lancet. 2015 Oct 3;386(10001):e16.
案例五、Lancet:“颈痛2月”——罕见寄生虫感染病例报道
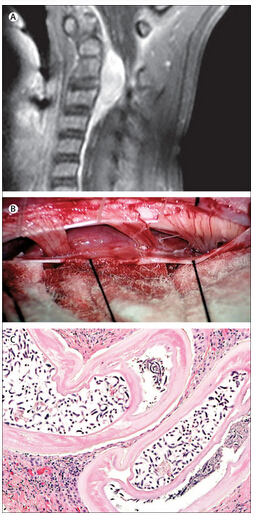
一名5岁21-三体女孩,颈痛2月,检查未发现神经系统异常和皮肤异常。MRI示C2-C4区域基于硬脑膜的肿块,导致脊髓受压。难道是周围神经鞘瘤或脑膜瘤?不过这类肿瘤在儿童是罕见的。后行了硬膜内肿块切除术。
组织病理学示:该肿块内包含一个,含丰富微丝蚴的怀孕的双子宫成年雌性线虫。显微镜下发现:角质层表面脊增厚,与盘尾属表现一致。
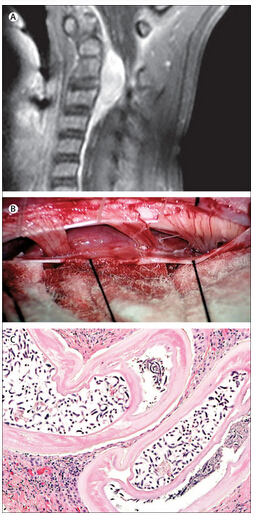
术后18天行腰椎穿刺脑脊液中没有发现微丝蚴,眼部检查也没有发现明显异常。
因担心体内还有微丝蚴,开始使用伊维菌素和强力霉素进行治疗。
9个月后患者临床表现和影像学检查均提示没有复发。
目前并不知道患者为什么会感染上该寄生虫。她住在新墨西哥州西北农村,经常去她家附近的纳瓦霍人湖。对她家的两只狗进行眼睛和皮肤检查,没有发现盘尾属感染的证据。她没有离开过美国,也没有被动物或昆虫咬伤史。
截至目前,全世界共报道了21例人畜共患盘尾属感染,关于盘尾属寄生虫(Onchocerca lupi)感染的仅仅只有5例。与本篇类似的报道有1篇,一名同地理区域的年轻女孩,表现为颈痛和上颈椎包块。
原始出处:Dudley RW, Smith C,et al.A cervical spine mass caused by Onchocerca lupi.Lancet. 2015 Oct 3;386(10001):1372.
组织病理学示:该肿块内包含一个,含丰富微丝蚴的怀孕的双子宫成年雌性线虫。显微镜下发现:角质层表面脊增厚,与盘尾属表现一致。
术后18天行腰椎穿刺脑脊液中没有发现微丝蚴,眼部检查也没有发现明显异常。
因担心体内还有微丝蚴,开始使用伊维菌素和强力霉素进行治疗。
9个月后患者临床表现和影像学检查均提示没有复发。
目前并不知道患者为什么会感染上该寄生虫。她住在新墨西哥州西北农村,经常去她家附近的纳瓦霍人湖。对她家的两只狗进行眼睛和皮肤检查,没有发现盘尾属感染的证据。她没有离开过美国,也没有被动物或昆虫咬伤史。
截至目前,全世界共报道了21例人畜共患盘尾属感染,关于盘尾属寄生虫(Onchocerca lupi)感染的仅仅只有5例。与本篇类似的报道有1篇,一名同地理区域的年轻女孩,表现为颈痛和上颈椎包块。
原始出处:Dudley RW, Smith C,et al.A cervical spine mass caused by Onchocerca lupi.Lancet. 2015 Oct 3;386(10001):1372.
案例六、JAMA子刊:什么是腹茧症?
患者男性,85 岁。因「恶心呕吐伴肛门停止排气排便 1 周」入院。患者诉腹痛轻微,既往有职业性石棉接触史,否认腹部手术史。
查体:腹部微隆,右下腹轻压痛。急诊予胃肠减压,引流出深色、恶臭胃内容物。
实验室检查显示白细胞 13000/ul。
腹部增强 CT 显示小肠广泛扩张(大于 4.7 cm),至末端回肠均可见气液平(图 1A、B)。结肠未见异常。
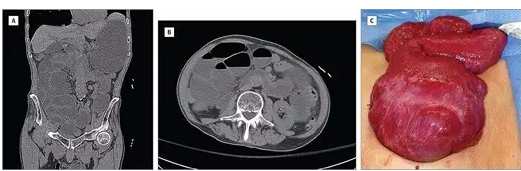
图 1. 腹部增强 CT 扫描(A、B)及术中所见(C)
予急诊行剖腹探查术。
术中发现,大部分小肠包裹在致密的粘连中(图 1C)。在这种情况下,考虑到肠袢分离难度较大,予切除粘连段肠管(约 110 cm),行端端吻合。
患者肠功能恢复迅速,术后第四天正常进食,出院。术后病理提示:小肠肠壁水肿、增厚,浆膜层外有致密的纤维组织包绕,无淀粉样蛋白沉积或抗酸菌感染迹象。
以上个案病例报道包括罕见病、疑难病、药物不良反应和疾病特殊临床表现。病例报告,包括单一的病例报告、两个案例报告或病例系列。发表病例报告可以描述被漏诊或未被发现的临床试验中重要的科学观测,并提供个性化的临床见解。
病例报告可以发挥下列功能:
(1)发现新疾病
系列病例报道案件可以发现潜在的新的疾病并引起公共的注意。其最常见的为对已有疾病的进一步分类。如尽管艾滋病病毒可能是在中部非洲超过百年的老病,只有当它在国际上传播后才被确认。
(2)疾病机制研究
病因线索可来源于病例报告。关于吸烟与肺癌关系的第一线索来自在20世纪20和30年代的手术病人系列,而正规的对照研究很晚才有。
(3)提出新的疗法
抗结核药物改善情绪导致新的抗抑郁药的应用等。
(4)识别副作用
有时副作用被发现是因为药物诱发了以前不存在或没有识别的症状。如没有其他任何促发因素下年轻女子在服用口服避孕药后几周发生静脉血栓。
Charlton and Walston建议将病例报道形式格式化,这样有利于以后文献整合。
通常情况个案报告应包括以下几个部分:
1)标题:标题是摘要的总结,让读者知道文章的重要性和相关性。
2)摘要:文章的主要信息应归纳在摘要内,因为这是读者会充分重视的部分。
3)引言:介绍为什么病例值得报告。
4)病例介绍: 病案应以简洁的时间顺序来描述。通常要开始于主诉,其次是家族史,职业病史,药物史或过敏史等,然后是身体检查结果连同相关的实验室和放射学结果。要有足够的细节让读者做出他们自己的判断。病人的后续进展和结果也应加以说明。并注意保护患者保密的隐私权。
5)讨论与建议:在讨论部分的目的是与已公开发表的文献病例报告进行比较;总结本病例报告的基本特征。至关重要的是有很好的文献复习。所有引用的参考文献应审慎评估。综述文章一般不是好的参考文献。列出一个表,以展示文献综述检的相关事实及详细的数据。牢记病例报告的局限性,笔者一定要小心,不要在有限的信息下轻易下判断和建议。(部分内容摘自王毅翔 氢思语)
德克萨斯大学健康科学中心表示,大多数期刊发表的病例报告大多具有以下特点:
• 不寻常发现
• 对治疗的不良反应
• 令人困惑的不寻常的综合症状
• 新理论的例证
• 现有理论的问题
• 个人影响
病例研究是全球医生分享自身处理困难病患经验的方式,这对临床医生来说是很有价值的参考信息和指引,尤其是遇到病患处在复杂困难的情况时。
以上四大期刊对案例报道筛选通常比较严格,除了做到稿件本身的质量外,还要求案例新颖,罕见或讨论独到能起到切实的临床指导作用;另外还有几个新的在线期刊专门在发表临床病例报告,比如BMJ Case Reports、Cases Journal、Journal of Medical Case Reports 和 Radiology Case Reports等。
临床医生在工作中要善于总结经验自然不说,在碰到疑难病例和罕见病例时更要长个心眼,一个不小心就有可能引发严重的后果。医生都是越做越小心。
曾在临床上碰到一个主任,对管床医生因放过一例疑似克罗恩病病人转院治疗后未进行跟踪随访,大发雷霆,连着叨叨了几天。这是主任对年轻医生的谆谆教导和殷切期盼,临床总是在不断积累和发现中前进的。对新现象的发现和归纳也是临床医生的一大乐趣,当然是风险与机遇并存的。吃一堑长一智是每个医生都必须不断经历的事,可能有些往往伴随着惨痛的教训。善于归纳和分享经验,做到举一反三,资源共享,是做医生的一大乐事,也是幸事。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







**被蛇咬
80
非常好,学习了。
137
值得学习
119
#医学期刊#
43
学习哒~~
131
涨知识
124
赞
78
赞
88
越来越精湛的技术
85
很现实的几个病例,受教了
111