PNAS:早期结直肠腺瘤生长相关的保守血清蛋白生物标志物
2019-04-12 海北 MedSci原创
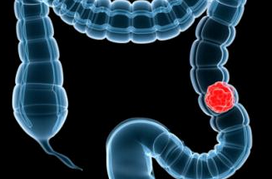
减少结肠癌的主要挑战是通过微创检测来检测携带高风险恶变前腺瘤的患者。 经过探索,研究人员已经解决了在携带最小线性尺寸小至6-9mm的腺瘤患者的血清中检测蛋白质信号的可行性。
减少结肠癌的主要挑战是通过微创检测来检测携带高风险恶变前腺瘤的患者。
经过探索,研究人员已经解决了在携带最小线性尺寸小至6-9mm的腺瘤患者的血清中检测蛋白质信号的可行性。
最近,研究人员在患者中使用定量质谱分析,对血清蛋白生物标志物进行了研究,这些标志物是在早期结肠腺瘤形成的两种动物模型中发现的。
一个队列包括已知在纵向计算机断层扫描结肠成像的基础上生长的患有腺瘤的患者。通过光学结肠镜检查筛选的另一组患者包括无腺瘤的患者和患有腺瘤的患者,其风险状态通过组织病理学进行判断。
在该患者研究和Pirc大鼠模型的研究中,标志物F5,ITIH4,LRG1和VTN均升高。 Pirc大鼠模型中的定量研究已经证明,这些标志物中每一种的升高水平与结肠腺瘤的数量相关。然而,患者中这些标志物的水平与总腺瘤体积没有显着相关性。
后息肉切除术血液样本证明,这四个保守标记物的水平升高在息肉切除术后持续存在。在息肉切除术后两个额外的血清标志物迅速重新正常化:生长相关的CRP水平仅在高风险腺瘤中增强,而与生长无关的PI16水平无论风险状态如何都降低。
最后,研究人员还形成了生物学假设,以解释这些观察结果,以及这些信号有助于预防结肠癌的方法。
原始出处:
Ivancic MM et al. Conserved serum protein biomarkers associated with growing early colorectal adenomas. PNAS, 2019; doi: 10.1073/pnas.1813212116.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#标志物#
23
#PNAS#
0
#结直肠#
30
#生物标志#
28
#生物标志#
28