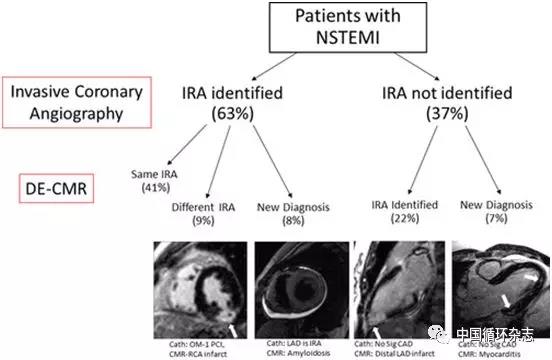
Circ Cardiovasc Interv:识别NSTEMI罪犯血管,心脏磁共振完胜冠脉造影
2019-05-16 卢芳 中国循环杂志
一项发表在Circulation子刊的前瞻性研究显示,就非ST段抬高型心肌梗死(NSTEMI)的罪犯病变发现而言,常规冠脉造影不敌延迟增强心脏磁共振成像(DE-CMR)。近1/3的NSTEMI患者,可通过磁共振识别出不同或新的罪犯病变。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
22
#NST#
36
磁共振心脏检查,很多医院做不了
60
#磁共振#
22
#心脏磁共振#
30
#冠脉造影#
41
#STEM#
0
#造影#
22
#NSTEMI#
0