Thyroid:NSAIDs不能降低甲状腺癌风险
2015-11-09 Seven L 译 MedSci原创
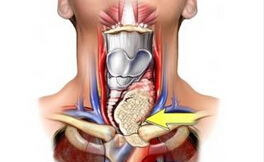
有研究报道环氧合酶(COX-2)与某些癌症的生长转移息息相关,其中就包括甲状腺癌。也有研究者探究了COX-2抑制剂对临床前甲状腺癌模型的影响,发现其具有抗肿瘤作用 。因此研究者进行了一项研究,探究使用非甾体类抗炎药 (NSAIDs)能否减少甲状腺癌的发生,以及探究甲状腺癌的危险因素或保护因素。该研究包含了3个大型的前瞻性研究,采集了参与者纳入研究前1年阿司匹林和其余NSAIDs的使用频率(未使用,
有研究报道环氧合酶(COX-2)与某些癌症的生长转移息息相关,其中就包括甲状腺癌。也有研究者探究了COX-2抑制剂对临床前甲状腺癌模型的影响,发现其具有抗肿瘤作用 。因此研究者进行了一项研究,探究使用非甾体类抗炎药 (NSAIDs)能否减少甲状腺癌的发生,以及探究甲状腺癌的危险因素或保护因素。
该研究包含了3个大型的前瞻性研究,采集了参与者纳入研究前1年阿司匹林和其余NSAIDs的使用频率(未使用 ≤2/周, >2-6/周,≥7/周),探究其与接下来甲状腺癌发生风险。
该研究共纳入388,577名患者,有 481例甲状腺癌发生。规律使用非阿司匹林NSAIDs的人群,并没有发现甲状腺风险的显著降低(HR 1.14, CI 0.84-1.55),阿司匹林同样不能减少甲状腺癌风险(HR 1.06, CI 0.82-1.39)。
研究者发现以下因素会导致甲状腺癌风险增加:女性、BMI在30-35.99之间。以下因素起保护作用:吸烟现状、少量饮酒。
NSAIDs不管是不是阿司匹林,均不能减少甲状腺癌风险。女性和肥胖会增加该疾病风险,相反吸烟喝酒却起着保护作用。
原始出处:
Patel DT, Kitahara CM,et al.Thyroid Cancer and Nonsteroidal Antiinflammatory Drug Use: A Pooled Analysis of Patients Over 40 years of Age.Thyroid. 2015 Oct 1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#癌风险#
44
#AID#
50
#SAID#
46
这篇文章有一定深度
130
是一篇不错的文章
192
值得进一步关注
165
不错,赞一个
111
赞
91
Mm
89
I'm
97