盘点:多发性骨髓瘤近期重要研究进展汇总
2018-05-27 MedSci MedSci原创
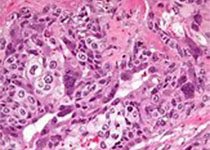
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里梅斯小编整理了近期关于多发性骨髓瘤的重要研究新进展与各位一同分享。
在美国,多发性骨髓瘤(骨髓瘤、浆细胞骨髓瘤)已成为仅次于淋巴瘤和白血病的最常见血液恶性肿瘤。骨髓瘤起源于骨髓造血组织,以浆细胞为主的恶性肿瘤,可以是孤立性,由于其产生多发性骨损害,故也称为多发性骨髓瘤,多发于40岁以上男性,好发部位依次为脊椎、肋骨、颅骨、胸骨等。目前,骨髓瘤被认为是可治愈性疾病,但用目前的治疗方法治愈率极低。这里梅斯小编整理了近期关于多发性骨髓瘤的重要研究新进展与各位一同分享。
【1】成年后体重指数、体力活动与多发性骨髓瘤风险
肥胖是唯一已知的可调节的多发性骨髓瘤(MM)危险因素。然而,在成年早期或晚期肥胖的影响以及其他能量平衡在MM发生发展中的作用尚不清楚。近日,近期一项研究中,研究人员反复利用护士健康研究、卫生专业人员随访研究和妇女健康研究小组的更新数据,进一步探讨MM病因中的能量平衡指标。该研究来自于调查问卷的暴露因素包括年轻成人体重指数(BMI)、累积平均BMI、年轻时BMI的变化以及累积的平均体力活动和行走距离。 研究人员观察到超过五百万人次每年的随访中共有575例MM患者。汇总分析发现成年早期和成年后较高的BMI是MM的危险因素。
【2】增强子活化和染色质聚散是原发性多发性骨髓瘤的调控网络
多发性骨髓瘤(MM)是一种起源于分泌抗体的浆细胞的侵袭性癌症。虽然现对其相关遗传和转录的特性已获得很好的了解,但该疾病相关的异常基因网络尚未得到充分的认识。现有研究人员在原发性MM细胞中绘制了调控元件、解旋的染色质和转录因子足迹。与分泌正常抗体的细胞相比,MM细胞表现为增强子活性持续改变,与超级增强子(SE)介导的转录因子(TF)基因异常调节相关。MM细胞还出现广泛的异染色质松散,与调控元件激活和部分患者的cAMP信号通路调控异常相关。最后,建立与SE相关的以TF为基础的调控网络可帮助识别一些对MM生物学至关重要的新的TFs。
【3】狄诺塞麦对比唑来膦酸治疗新确诊的多发性骨髓瘤患者的骨骼症状的效果对比
狄诺塞麦(denosumab)是一种靶向RANKL的单克隆抗体,可减轻多发性骨髓瘤晚期实体肿瘤患者骨溶解或骨转移相关的骨症状。一项国际性的双盲双模拟的随机化活性对照的3期研究评估了狄诺塞麦与唑来膦酸相比,用于新确诊的多发性骨髓瘤患者预防其骨骼相关症状的效果和安全性。招募年满18岁的新确诊的有症状的至少有一处溶骨性损伤的多发性骨髓瘤患者,按1:1随机分至狄诺塞麦(120mg 皮下注射)联合安慰剂组或唑来膦酸(4mg)联合安慰剂,每4周一次。结果显示,对于新确诊的多发性骨髓瘤患者,狄诺塞麦延缓发生骨骼相关症状时间的效果,不劣于唑来膦酸。本研究结果表明狄诺塞麦或许可作为有骨骼症状的多发性骨髓瘤患者标准疗法的补充治疗。
【4】Daratumab、硼替佐米、马法兰和强的松有望成为不可移植多发性骨髓瘤患者的一线治疗方案
对于不可接受自体干细胞移植的新发多发性骨髓瘤患者,硼替佐米、马法兰和强的松的联合治疗是该类患者的标准治疗方案。Daratumab联合标准治疗对复发性或难治性多发性骨髓瘤具有较高的疾病缓解效果,近日一项III期临床研究探究了Daratumab联合标准治疗一线治疗不能接受干细胞移植的新发多发性骨髓瘤患者的疗效。研究招募了706名新发不可接受干细胞移植的多发性骨髓瘤患者,随机接受9轮标准治疗方案化疗或Daratumab联合标准治疗方案。平均随访16.5个月,Daratumumab组18个月无进展生存率为71.6%,对照组为50.2%。Daratumab治疗总缓解率为90.9%,对照组为73.9%,组间完全响应,包括严格的完全响应率分别为42.6%和24.4%。Daratumab组中,22.3%的患者微小疾病残留阴性,对照组为6.2%。研究认为,Daratumumab联合标准治疗方案治疗不可接受干细胞移植的新发多发性骨髓瘤患者的效果优于标准治疗方案。
【5】Carfilzomib治疗多发性骨髓瘤或增加CVD风险
近日,来自美国宾夕法尼亚大学的研究人员对24项前瞻性临床试验共包括2594例患者数据进行系统性综述和荟萃分析。24项研究均有高级别的CVAE数据,22项研究有所有级别的CVAE数据。结果发现,不可逆蛋白酶体抑制剂carfilzomib与临床相关的不良心血管疾病(CVD)事件风险相关,包括高级别(high-grade)心血管不良事件(CVAEs),carfilzomib之前被批准用于治疗多发性骨髓瘤(MM)。表明MM患者人群CVAE基线风险高,MM患者关注心血管风险治疗很重要。护理MM患者的临床医生必须注意CVAE的早期征象,并及时对这些患者进行进一步的评估。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#多发性#
32
谢谢分享
51
谢谢分享
37
#研究进展#
27
学习了.谢谢分享.
52
好知识值得借鉴!!
48