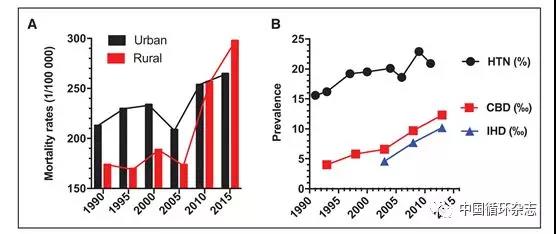
Eur Heart J:稳定性冠心病患者血压应<140/80 mmHg
2018-08-26 朱柳媛 中国循环杂志
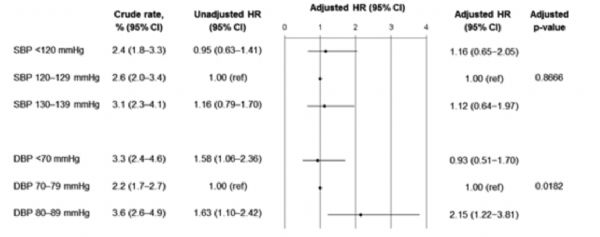
2017年美国高血压新指南发布至今,争议不断。其一是将高血压重新定义,即将平均收缩压>130 mmHg或舒张压>80 mmHg作为高血压诊断标准,此前相应的标准是140/90 mmHg。更有争议的是,只要血压>130/80 mmHg,该指南都建议接受降压治疗。根据这个新指南,收缩压处于130~139mmHg或舒张压80~89 mmHg的冠心病患者都要服用降压药物,而这部分人按照既
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#稳定性#
31
#ART#
23
#冠心病患者#
28
#HEART#
31