JCI & CHEST J:端粒突变更易患肺部疾病
2015-02-10 佚名 生物谷
近日,刊登在国际杂志Journal of Clinical Investigation及CHEST Journal上的两篇研究论文中,来自杨百翰大学的研究者表示,他们知道我们中的大部分人什么时候死亡?但研究者并不不清楚我们确切的死亡事件,当然他们得出这样的结论得益于对我们机体染色体生物钟的研究,染色体末端的端粒可以帮助预测机体的寿命,其越短就表示我们寿命越短。 较短的端粒可以帮助预测骨髓衰竭、肝
近日,刊登在国际杂志Journal of Clinical Investigation及CHEST Journal上的两篇研究论文中,来自杨百翰大学的研究者表示,他们知道我们中的大部分人什么时候死亡?但研究者并不不清楚我们确切的死亡事件,当然他们得出这样的结论得益于对我们机体染色体生物钟的研究,染色体末端的端粒可以帮助预测机体的寿命,其越短就表示我们寿命越短。
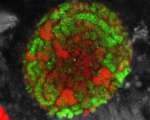
较短的端粒可以帮助预测骨髓衰竭、肝脏疾病、皮肤及肺部疾病等;研究者在过去30年里一直从事端粒的相关研究,他们试图利用方法来延伸端粒,并且研究端粒的相关突变,而如今研究者发现了端粒和肺部疾病的关联。Alder教授说道,当我们出生时,我们的端粒非常长,随着年龄增长端粒会不断变短,本文中我们发现肺部疾病的个体端粒往往相比正常个体的端粒较短。
端粒是染色体的保护性帽子,就好象是鞋带儿上的塑料帽一样保护鞋带,当细胞分裂复制一次,端粒末端的DNA就会减少,因此在人的一生中随着细胞不断分裂,染色体末端的端粒就会不断变短。当端粒耗尽细胞就会失活或者死亡,从而引发疾病。某些科学家发现了可以延长端粒的方法,但这并不总是好的,因为维持长度的端粒往往也会引发并发症,比如癌症等疾病。
文章中,研究者发现,发生肺气肿的部分患者机体中在维持端粒的基因上往往会发生一些突变;如果已知端粒基因突变会引发肺纤维化,那么本文的研究就可以将端粒和肺部疾病相关联起来。端粒突变的家族会将这些遗传突变遗传给厚道,这就会导致后代也会携带较短的端粒,而携带较短端粒的个体或患肺部疾病的风险较高。
最后,研究者Mary Armanios指出,大部分人并不会意识到肺部疾病是引发美国人死亡的常见三大原因,而对端粒的研究或许对于预防肺部疾病也具有一定的指示意义;我们都知道吸烟者往往患肺部疾病的风险较高,本文研究或许也可推理出,吸烟的端粒突变个体往往患肺部疾病的风险或更高。
原始出处
Stanley SE, Chen JJ, Podlevsky JD, Alder JK, Hansel NN, Mathias RA, Qi X, Rafaels NM, Wise RA, Silverman EK, Barnes KC, Armanios M.Telomerase mutations in smokers with severe emphysema.J Clin Invest. 2015 Feb;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#EST#
23
#Chest#
21
#JCI#
23
以阅
112
#肺部疾病#
21