EuroPCR2018丨临界冠脉狭窄患者易损斑块OCT特征的临床结局
2018-05-27 国际循环编辑部 国际循环
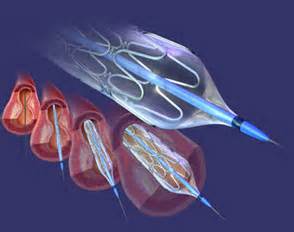
既往研究显示,某些光学相干断层扫描(OCT)特征如薄纤维帽粥样斑块(TCFA)可增加不良事件发生率。EuroPCR 2018大会上,波兰华沙医科大学 TOMANIAK M.等研究者发表一项最新研究结果,旨在确定在经血流储备分数(FFR)证实不明显的、血管造影所示的临界冠状动脉病变患者易损斑块OCT特征与随访1年临床结局的相关性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床结局#
33
#OCT#
30
#冠脉狭窄#
30
#EuroPCR#
28
#斑块#
29
#PCR#
29
学习了.感谢分享.
54
感谢分享.
66
不错的文章值得学习到了.
74
学习一下谢谢
64