J Hypertens:心内科高血压患者有1/3患糖尿病,内分泌科糖尿病患者有2/3合并高血压
2016-12-28 卢芳 中国循环杂志
由上海瑞金医院王继光等进行的研究显示,高血压和糖尿病共患率较高,但对于心内科和内分泌科而言,前来就诊的二病并存患者,前者控糖药物使用不够,后者降压药物使用不足,血压血糖均达标者两科均不过半。 研究者指出,或许高血压和糖尿病联合管理平台有助于提高和改善当前救治状况。 研究显示,在心内科就诊的高血压患者约有1/3同时罹患糖尿病,而在内分泌科就诊的糖尿病患者中则有约2/3合并高血压。
由上海瑞金医院王继光等进行的研究显示,高血压和糖尿病共患率较高,但对于心内科和内分泌科而言,前来就诊的二病并存患者,前者控糖药物使用不够,后者降压药物使用不足,血压血糖均达标者两科均不过半。
研究者指出,或许高血压和糖尿病联合管理平台有助于提高和改善当前救治状况。
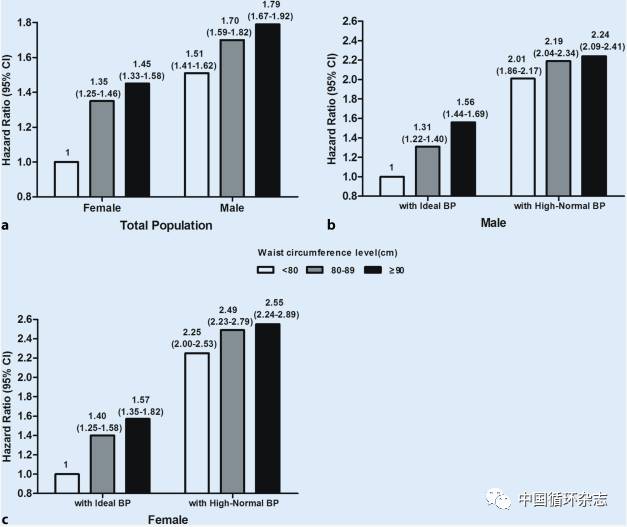
研究显示,在心内科就诊的高血压患者约有1/3同时罹患糖尿病,而在内分泌科就诊的糖尿病患者中则有约2/3合并高血压。总体受试者中,有45.3%二病共患(图1)。

图1 在心内科和内分泌科高血压和糖尿病共患流行状况
在高血压管理方面,当前无论是高血压临床管理指南,还是糖尿病指南相关推荐,均指出,对于二病共患者,要严格控制血压,并且肾素-血管紧张素系统抑制类降压药为一线降压药。
但研究者进一步分析发现,在内分泌科,降糖时联合应用降压药治疗(25.1% vs 51.5%),以及应用肾素-血管紧张素系统抑制类降压药(46.7% vs 56.9%)比例均低于心内科。
而在心内科,对于二病共存患者,降压时联合应用口服降糖药或胰岛素使用比例低于内分泌科(4.2% vs 21.2%)。
不过,比较两类科室,不论是140/90 mmHg还是130/80 mmHg为降压目标,还是糖化血红蛋白以7.0%或6.5%为降糖目标,二病共患者其血压、血糖控制率均无统计学差异。
糖尿病和高血压共患时,多会增加肾病风险。研究也显示,二病共患者其蛋白尿罹患率为23.3%,而仅有高血压者为12.6%,仅有糖尿病者为15.9%。而且,蛋白尿随着血压、血糖的升高而患病率也升高。研究者认为,这支持二病共患者130/80 mmHg为降压目标更适宜。
这项横断面多中心研究共纳入2459例就诊者,包括在心内科就诊的1291例高血压患者,和在内分泌科就诊的1168例糖尿病患者。
原始出处:
Song J, Sheng CS, Huang QF, et al. Management of hypertension and diabetes mellitus by cardiovascular and endocrine physicians: a China registry. J Hypertens, 2016, 34: 1648-53.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
21
#分泌#
39
#TENS#
34
#心内科#
39
#高血压患者#
30
#糖尿病患者#
23
内分泌及不合格的相互交叉性
70