Sci Rep:肥胖节食男性中,睾丸素治疗对骨重建标记和矿物密度的影响研究
2018-06-24 AlexYang MedSci原创
最近,有研究人员在节食肥胖男性中,评估了睾丸素治疗对骨重建和密度的影响。研究包括了100名肥胖男性,平均年龄为53岁(范围为47-60岁),并且他们的总睾丸素水平<12nmlol/L,并接受为期10周的低能量饮食(VLED)。另外,他们进行了为期46周的体重保持,并被随机分配到基点到56周的肌肉内注射十一酸睾酮(n=49)或者匹配的安慰剂组(n=51)。在两组之间预先确定的差异结果(平均调整
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#骨重建#
28
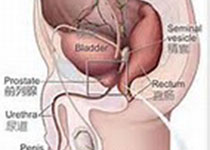
#睾丸#
27
#节食#
24
#睾丸素#
22
一起学习学习
47