J Urban Health:艾滋病毒传播与种族/民族/地域差异之间的联系
2017-09-29 佚名 Medical Xpress
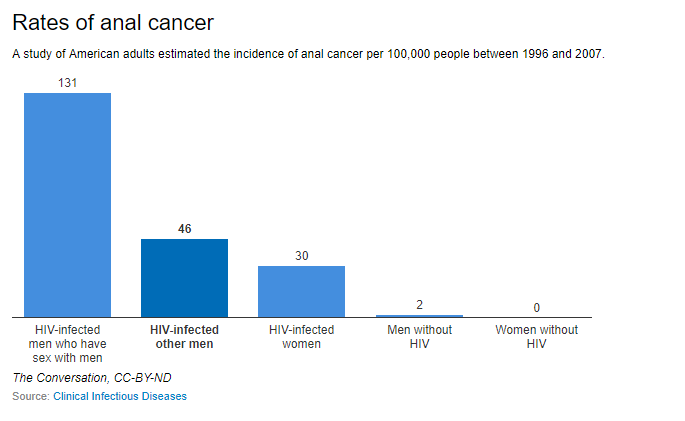
人们生活,工作和健康有很好的记录,以及旨在改善健康的邻里级结构性干预措施有很大的价值。但是,导致艾滋病毒传播和疾病负担差距的基于地方特征的了解甚少,这可能导致减少艾滋病毒的干预措施和计划编制效率低下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习学习.继续关注
90
继续学习中谢谢
82
#Health#
34
#ALT#
24
好好努力学习
81
不错的文章值得推荐一下了
65