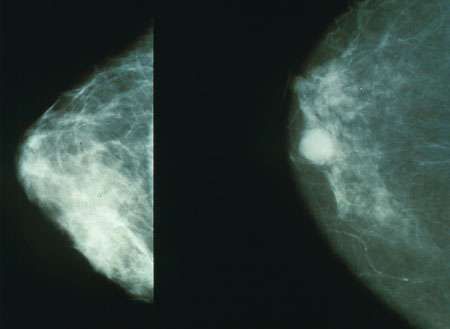
CLIN CHEM:在新辅助化疗过程中检测三阴性乳腺癌患者的特异性循环肿瘤DNA
2017-03-27 MedSci MedSci原创
近日,来自意大利蒙扎San Gerardo医院肿瘤科报道了一项关于在新辅助化疗过程中检测三阴性乳腺癌患者的特异性循环肿瘤DNA的研究, 相关研究成果刊登于国际杂志CLIN CHEM上。 在非转移性三阴性乳腺癌(TNBC)患者中,研究人员研究了循环肿瘤DNA(ctDNA)检测是否可以反映新辅助化疗(NCT)的肿瘤反应,并检测手术后的最小残留病变。 研究人员在4个时间点收集10毫升血浆:NCT前;
近日,来自意大利蒙扎San Gerardo医院肿瘤科报道了一项关于在新辅助化疗过程中检测三阴性乳腺癌患者的特异性循环肿瘤DNA的研究, 相关研究成果刊登于国际杂志CLIN CHEM上。
在非转移性三阴性乳腺癌(TNBC)患者中,研究人员研究了循环肿瘤DNA(ctDNA)检测是否可以反映新辅助化疗(NCT)的肿瘤反应,并检测手术后的最小残留病变。
研究人员在4个时间点收集10毫升血浆:NCT前; 1周后;手术前手术后。使用定制的液滴数字PCR(ddPCR)测定法通过大规模平行测序(MPS)跟踪先前在肿瘤组织中特异性表达的肿瘤蛋白p53(TP53)突变。
研究结果显示:46例非转移性TNBC患者入组。其中40例鉴定出TP53突变。定制的ddPCR探针对38例患者进行了验证,与MPS(r = 0.99),特异性(≥2滴/测定)和灵敏度(至少为0.1%)具有良好的相关性。在基线时,36例中的27例患者检测到ctDNA(75%)。其检出与有丝分裂指数(P = 0.003),肿瘤分级(P = 0.003)和分期(P = 0.03)有关。在治疗期间,我们观察到所有患者的ctDNA水平下降,但1.手术后没有患者检测到ctDNA。 ctDNA水平升高的患者在NCT期间经历肿瘤恶化。病情完全缓解(16例)与任何时间点的ctDNA检测无关。 NCT 1周期后的ctDNA阳性与短期不发病(P <0.001)和总体(P = 0.006)的生存期相关。
研究发现,定制ctDNA检测可以达到75%检测率。在NCT期间,ctDNA水平迅速下降,手术后未检测到残留病变。然而,NCT期间ctDNA水平的缓慢下降与较短的存活期密切相关。
原始出处:
Francesca Riva, Francois-Clement Bidard,
Alexandre Houy. et al. Patient-Specific Circulating Tumor DNA Detection during
Neoadjuvant Chemotherapy in Triple-Negative Breast Cancer. DOI:
10.1373/clinchem.2016.262337 Published February 2017
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特异性#
46
#新辅助#
47
#阴性乳腺癌#
38
#三阴性#
32
#循环肿瘤DNA#
32
#乳腺癌患者#
36
非常好的文章
77