股骨头坏死的保头治疗进展
2016-10-18 河南省中医院 孙永强 风湿病与关节炎2016年9月第5卷第9期
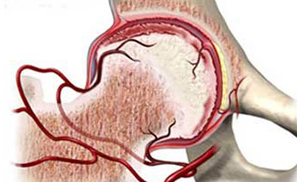
股骨头坏死(ONFH)是骨科临床常见疾病之一,多见于中青年,主要分布在20~50 岁人群,其中双侧病变占60%以上,男女患病比例约为4:1。目前,本病的主要发病机制尚未明确,由于股骨头血供受损,血液供应不足,诱发骨细胞和骨髓成分死亡,在骨细胞修复的时候由于新骨应力不足,患肢负重,新骨区因受力而出现结构改变,股骨头发生微骨折,最后导致塌陷。临床症状表现为腹股沟处疼痛,髋关节功能障碍,甚至站立及行
股骨头坏死(ONFH)是骨科临床常见疾病之一,多见于中青年,主要分布在20~50 岁人群,其中双侧病变占60%以上,男女患病比例约为4:1。目前,本病的主要发病机制尚未明确,由于股骨头血供受损,血液供应不足,诱发骨细胞和骨髓成分死亡,在骨细胞修复的时候由于新骨应力不足,患肢负重,新骨区因受力而出现结构改变,股骨头发生微骨折,最后导致塌陷。临床症状表现为腹股沟处疼痛,髋关节功能障碍,甚至站立及行走困难等。在临床上,根据ONFH 分期不同,可采取保守治疗或手术治疗,当股骨头塌陷严重时就不得不采取人工关节置换术(THA);但术后可能出现假体磨损和松动等严峻问题,患者需要面临二次甚至多次翻修,这将会给患者和家属带来巨大的压力和痛苦。因此保留患者的股骨头是治疗早期ONFH的根本目的,故早期发现和诊治十分重要。近年来随着医学的不断发展,采取有效方法可以延缓或阻止股骨头塌陷,从而推迟或避免THA。现就ONFH 的保头治疗进展作一综述。
非手术治疗
早期ONFH,可以通过口服药物、理疗、限制性负重、冲击波、针灸、针刀等治疗取得一定的临床效果,从而达到延缓或者治愈早期ONFH的目的。
限制性负重:包括部分负重和完全不负重,必要时需要绝对卧床。ONFH 处在新旧骨交替的过程,骨应力比正常骨小,下肢负重大大增加了股骨头微骨折的概率,有效的不负重休息有利于股骨头水肿的自我代谢和吸收。Zaino 等指出,治疗ONFH 时应该特别重视股骨头前半球,因为它是主要负重部位,非常容易发生病变。单一的依靠限制负重治疗早期ONFH的临床效果并不理想,目前临床应用较少。Okazaki 等通过小鼠实验指出,不负重并不能阻止股骨头坏死的进一步发展。可见限制性负重或免负重可以有效预防股骨头变形塌陷,但并不能阻止坏死病变的发展。
药物治疗
中药治疗 ONFH 属中医学“骨痹”“骨蚀”范畴。中医学认为,痰、湿、瘀是引起本病的主要因素,痰湿为标,肾虚为本,血瘀是标本共同产物,故治疗以补肾、祛痰湿、活血化瘀为原则。唐宗海在《血证论·吐血》中指出:“气为血之帅,血随之而运行,血为气之守,气得之而静谧。”魏秋实等将91例133髋ONFH患者根据临床症状分为气滞血瘀型、肾虚瘀血型、痰瘀蕴结型,分别为31例41髋、37例56髋、23例36髋;按ARCO分期为Ⅰ期11 髋,Ⅱ期43 髋(根据CT是否存在软骨下骨折,分为稳定型31 髋和不稳定型12 髋),Ⅲ期58 髋,Ⅳ期21 髋,经过中药对应治疗后,其生存率分别为Ⅰ期100%,Ⅱ期(稳定型)96.8%,Ⅱ期(不稳定型)75.0%,Ⅲ期67.2%,Ⅳ期61.9%。Wang 等给予壮骨丸治疗小鼠ONFH,结果表明,壮骨丸能够改善血液循环,促进新骨生成,加速死骨修复,且无不良反应。中药治疗可以通过滋补肝肾、活血化瘀、祛痰除湿等方法改善患者机体体质,从而延缓病程或者治愈早期ONFH。
西药治疗 现代医学认为,导致ONFH 的因素有静脉血栓形成、脂肪栓塞、骨内压增高、成骨减弱、破骨增强等,因此临床上常运用扩血管药、降脂药、抗凝药、双膦酸盐等治疗ONFH。陈占斌等通过临床观察指出,运用美多巴治疗ONFH 临床满意率达75.34%,可以有效延缓人工关节置换的时间。康鹏德等运用抗凝药(华法林)、降脂药(洛伐他汀)治疗激素型ONFH 兔子68只,洛伐他汀和华法林组、华法林组、洛伐他汀组和对照组,治疗12周,其骨坏死发生率分别为13.3%、35.3%、41.2%、68.8%。
物理治疗 物理疗法包括体外震波、鸡尾酒疗法、高频电场、磁疗、高压氧等,可以起到缓解疼痛和促进骨修复的作用。Vulpiani 等对36例ONFH 患者应用体外冲击波治疗,随访2 年,根据ARCO分期,结果显示,Ⅰ期、Ⅱ期疗效明显优于Ⅲ期,其中Ⅲ期患者66.7% 改行关节镜术。动物实验结果表明,体外冲击波疗法可以提高血管生长因子(如内皮型一氧化氮合酶、血管内皮生长因子、增殖细胞核抗原)的表达,从而促进血管形成。Camporesi 等通过临床观察认为,高压氧疗法治疗Ficat Ⅱ期ONFH患者有效。Hsu等认为,鸡尾酒疗法治疗早期ONFH 有效。
手术治疗
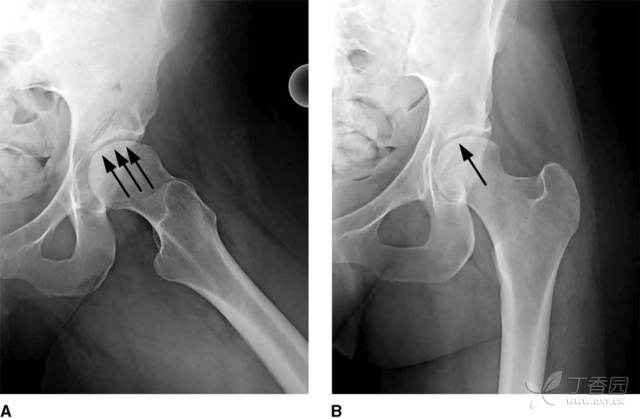
髓芯减压(CD) CD 最初被Ficat 和Arlet 应用于ONFH 的诊断中,该方法源于ONFH 股骨头髓芯穿刺获得标本的偶然发现。其原理是通过降低股骨头内高压,改善局部血液循环,促进血管和新骨生成。姬树青等将Steinberg 分期Ⅰ、Ⅱ期的ONFH 患者13 例(16 髋),采用小切口髓芯加压联合打压植骨并再次钻孔减压术治疗,Harris评分由术前(65.32±10.27)分变为术后12 个月(91.15±7.28)分,且X线示骨坏死区无进展,无塌陷出现。对于Ⅰ、Ⅱ期的患者CD 可减轻骨内压,促进血液循环,从而保持髋关节的稳定,延长髋关节置换时间。目前,CD 治疗早期ONFH尚存在一定的争议;但其操作简单,损伤小,恢复快,容易被患者接受;即使手术失败,后期可以采用其他手术治疗,故该方法在临床上一直应用至今。
骨移植 骨移植治疗ONFH 是指通过聚集有成骨潜能的细胞在局部诱导新骨生成,从而达到对股骨头支撑的效果,防止在修复期股骨头出现塌陷的现象,并且提高再血管化进程的速度。自体骨是骨移植的主要细胞来源。骨移植主要包括非血管化骨移植和血管化骨移植。
非血管化骨移植 非血管化骨移植原理:减压股骨头坏死区域,去除坏死骨组织,并植入具有骨诱导或骨传导的材料,达到支撑软骨下骨的作用。根据开窗部位不同将其分为以下3 种:①经股骨头关节软骨开窗植骨,并复位开窗软骨;②经股骨颈到股骨头基底部开窗植骨;③经股骨颈和头的髓芯减压隧道。Rosenwasser 等通过在股骨颈开窗、灯泡状清除坏死骨后并植入自体松质髂骨,随访10~15 年,其成功率达87%。康鹏德等回顾性分析钻孔减压基础上自体松质骨植入结合同种异体腓骨移植治疗早期ONFH(塌陷前期)16 例(16 髋),平均随访14 个月,结果Harris 评分由术前74 分提高到末次随访时的85 分。
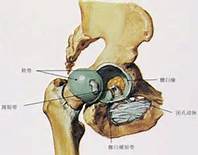
血管化骨移植 指把带有血管的骨组织植入股骨头坏死区域,提供血运,从而达到治疗ONFH 的目的。主要有2 种方式:①带血管蒂的骨移植;②吻合血管的游离骨移植。Elmali 等采用带血管蒂髂骨移植治疗ONFH患者22 例26 髋,其中Ⅱ期11 髋,Ⅲ期15 髋,术后平均随防36 个月,结果Harris 评分由术前52 分变为术后82.8 分,优良率为69%。Judet 等治疗股骨头血管性坏死应用吻合血管的游离腓骨移植(FVFG),结果术后经长期随访,成功率达75%~90%。de Ridder等在回顾200 例实施FVFG 的患者过程中发现,患者出现短暂性的感觉缺失,考虑是手术损伤了股外侧皮神经引起的。在手术过程中需要把关节囊切开,在此过程中容易导致关节粘连,后期可能出现关节功能障碍;但通过手术可以有效降低关节内压力及血管压力,从而减少股骨头坏死的机率。
钽棒植入 钽棒植入技术是以髓芯减压为基础,植入多孔钽棒,从而达到支撑股骨头和软骨下骨,促进新生血管和骨长入。多孔钽棒生物相容性很高,其表面为蜂窝状,孔隙率接近人体松质骨,弹性介于皮质骨和松质骨之间,能提高骨长入并降低应力遮挡,给骨组织修复提供良好的条件,对于即将塌陷的股骨头具有很好的支撑作用,其蜂窝状表面也利于骨长入。Floerkemeier 等采用钽棒植入治疗19 例(23髋)ONFH 患者,平均随访592d,结果股骨头存活率为44%,最后11例(13髋)接受THA。张庆等采用Meta 法分析多孔钽棒治疗ONFH,得出钽棒治疗早期ONFH安全性高,并且给髓芯减压后支撑软骨板提供了一种微创手段。虽然钽棒植入技术优点很多,但该方法的安全性并不是100%,它也存在一定的风险。Floerkemeier等发现,钽棒植入会明显增加转子下区应力,增加骨折风险,MRI 检查示钽棒周围缺乏完全的骨长入。钽棒植入治疗ONFH 兼顾了股骨头内环境和机械支撑的问题,可阻止患者股骨头进一步塌陷,临床应用广泛。
截骨术 早期ONFH 的病位常在股骨头的前上部,股骨头后部的外形往往完整,且具有正常的软骨面及带血运的软骨下骨。通过截骨改变股骨头主要负重区,改变负重力线,改为正常骨替代坏死骨,阻止关节面进一步塌陷,为坏死区修复创造条件。而且,截骨可以开放髓腔,有效降低骨内压,并改善股骨头血供。Ito 等采用转子间内翻截骨术治疗28 例(34 髋)ONFH 患者,平均随访18.1 年,结果临床预后较满意。Ikemura 等采用经转子前旋转截骨治疗23 例(28 髋)年轻(≤ 20 岁)ONFH 患者,结果满意率为92.6%。截骨术并不是适应所有的早中期ONFH 患者,它也存在一些严重的手术并发症,如创伤大、恢复慢、患肢短缩等缺点。而且后期行THA 时,会增加手术难度,故临床应用较少。
细胞治疗 细胞治疗作为发展起来的一项技术应用在ONFH 的治疗中,由于各种低分化的细胞具有良好的生长活性,清除股骨头坏死病灶后,多遗留空腔,将具有分化能力的干细胞植入坏死区域,诱导新骨细胞生成分化,从而恢复股骨头血供并修复骨坏死。Wang 等采用清除死骨、植入自体皮松质骨和骨髓单核干细胞(含有MSCs)治疗ARCO Ⅱ~Ⅲ期ONFH 患者15 例(20 髋),平均随访24 个月,结果Harris 评分由术前65 分增至术后85 分,总成功率达80%。Mao 等采用介入灌注自体骨髓基质干细胞治疗78 髋患者,结果效果满意72 髋,Harris 评分提高明显。但目前干细胞治疗ONFH 尚存在一些问题,其安全性和有效性临床报告不一,存在较大差异,临床也无统一的评价方法与标准。
问题与展望
ONFH 的临床分型和治疗方法虽然很多,但针对每期ONFH 尚未有一种治疗效果十分明确的方法。故临床准确的分型和准确的治疗方法对治疗早中期ONFH 至关重要。只有有效地把握患者疾病程度,选择适合该程度的治疗方法,才能取得满意的临床效果。在保守治疗方面,中西药物各有其优劣之处,对于早期非手术治疗ONFH,综合应用中药和西药的优势,配合物理疗法等往往可以取得更好的临床效果。
手术保髋治疗有髓芯减压、骨移植、钽棒植入、截骨术、干细胞治疗等,每种方法各有其优点和缺点,只有严格把握手术适应证和并发症,才能取得满意手术效果。其中髓芯减压术具有手术创伤小、恢复快、操作简单等优势;但单纯的髓芯减压目前临床效果不一,临床上往往联合植骨或其他内植物综合治疗。带血管骨移植可以给坏死股骨头区提供血液,重建血运;而不带血管骨移植通过诱导作用从而达到机械支撑软骨下骨的效果。但自体骨移植需要取自患者身上,往往伴随着巨大的创伤,而异体骨存在组织相容性和感染问题。
钽棒具有生物相容性好,利于骨长入,有效支撑股骨头等优点;但存在假体周围骨折的风险。截骨术通过截骨后用正常股骨头区替代坏死区域,给坏死区修复创造条件达到治疗ONFH 的作用;但它存在创伤大、恢复慢、后期行THA 时增加手术难度等缺点。干细胞具有良好的生长活性和分化能力,可以诱导新骨细胞生成分化而达到恢复股骨头血供并修复骨坏死的效果,临床应用前景广阔,一直是骨科研究的热门话题;但其临床有效性和安全性差别大,需进一步深入研究。
早期THA 的患者可能面临后期二次或者多次翻修可能,这将给患者和家属的身心以及经济方面带来巨大的负担,因此有效的保髋对于延缓或阻止THA 十分重要。笔者希望通过本文总结目前治疗ONFH 保髋的一些常用方法和临床效果,给临床上治疗ONFH 提供参考。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#骨头#
37
感谢了
52
感谢介绍
60
感谢推荐
62
#坏死#
46
#股骨#
29
#股骨头#
38
这病据说跟饮酒有关!
66