JACC:巨大肺动脉瘤压迫左主干一例
2013-05-14 JACC dxy
70岁老年男性,23岁时意外诊断为特发性肺动脉扩张但一直无症状。一年前患者因阵发性房颤时心绞痛发作入院,快心室率时患者心电图提示ST段压低。冠脉造影提示左主干(LMCA)轻度狭窄。当时,平均肺动脉压力为36mmHg。回复至窦性心律后,患者临床症状消失,出院并长期使用β受体阻滞剂。一年后,患者因心绞痛再发入院。心脏超声和CTA提示动脉瘤扩大至80mm并压迫LMCA。冠脉造影证实了上述发现,血管内超声
70岁老年男性,23岁时意外诊断为特发性肺动脉扩张但一直无症状。一年前患者因阵发性房颤时心绞痛发作入院,快心室率时患者心电图提示ST段压低。冠脉造影提示左主干(LMCA)轻度狭窄。当时,平均肺动脉压力为36mmHg。回复至窦性心律后,患者临床症状消失,出院并长期使用β受体阻滞剂。
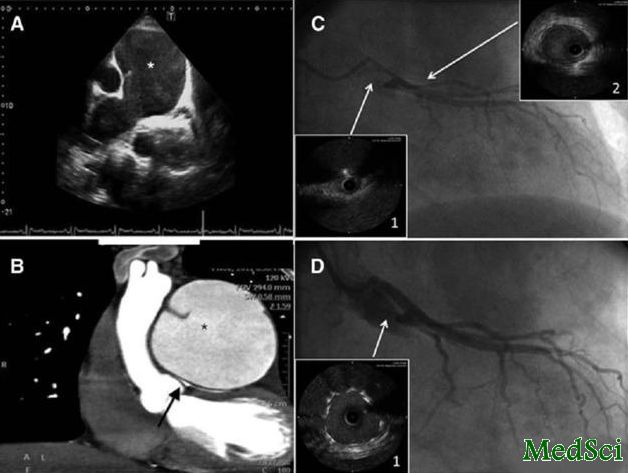
一年后,患者因心绞痛再发入院。心脏超声和CTA提示动脉瘤扩大至80mm并压迫LMCA。冠脉造影证实了上述发现,血管内超声提示LMCA重度狭窄,前降支管腔内径正常。平均肺动脉压力上升至>60mmHg。
由于外科手术风险高,患者接受了经皮LMCA血管成形术,植入药物涂层支架。并使用针对肺动脉高压的磷酸二酯酶-5抑制剂和内皮素受体拮抗剂。患者症状消失,出院门诊随访根据临床情况、肺动脉高压演变再次评估行动脉瘤切除术的指征。一年后患者无不良事件无症状。
LMCA外壁受到肺动脉瘤压迫的情形非常罕见,通常与肺动脉高压并存。仅有少量病例报告和小序列研究将此情形作为心绞痛和猝死的原因之一,目前对此类患者的适合治疗方式仍不清楚。
高分辨率CT使对于肺动脉瘤和LMCA压迫程度的评估成为可能。在本例中,血管内超声证实了诊断。
尽管其发生原因仍不清楚,但对有症状、并发症风险高的肺动脉瘤患者(动脉瘤>60mm、肺动脉高压)应行外科手术治疗。但同时,这也是一项高风险的手术,尤其是严重肺动脉高压机LMCA严重狭窄时。另外还有学者认为对严重LMCA阻塞的患者应行冠脉成形术。也有学者认为缩减肺动脉瘤大小后,能减轻LMCA压迫。
目前,主动脉冠脉旁路和无保护左主干支架植入是可选治疗方案,由于肺动脉高压患者外科手术风险高,更倾向于选择LMCA支架植入术,已有此类患者成功治疗的报道。需指出的是,这些发表的病例为开口或LMCA近端压迫、非分叉、仅需一枚支架处理。也有报道说,在不能耐受外科手术介入治疗风险也高的患者,在强化针对肺动脉高压的治疗后,压迫缓解。在类似本例的患者,存在不可避免的外科手术风险和引起症状的严重LMCA狭窄,经皮血管成形和强化肺动脉高压治疗可能是较合理的处理策略。
与肺动脉相关的拓展阅读:
- Chest:运动训练可提高肺动脉高压患者的心肺功能和生活质量
- JAMA IM:1/3肺动脉高压往往被错误诊断
- Circulation:伊马替尼治疗肺动脉高压风险获益并存
- Circulation:曲罗尼尔有望成为肺动脉高压一线治疗药物
- AM J RESP CRIT CARE:社会经济地位与肺动脉高压全因死亡率呈负相关 更多信息请点击:有关肺动脉更多资讯

Compression of the left main coronary artery by a giant pulmonary artery aneurysm.
We present a 70-year–old man who had a past medical history of dilated idiopathic pulmonary artery, incidentally diagnosed at the age of 23 years. He was asymptomatic until a year ago when he was admitted for an episode of anginal chest pain in the context of paroxysmal atrial fibrillation. At rapid rates, he showed pathological ST segment descent. A coronary angiography showed a slight stenosis of the left main coronary artery (LMCA). At that time, the mean pulmonary artery pressure was 36 mm Hg. After recovering sinus rhythm, the patient became asymptomatic and was discharged with β-blockers.
A year later, the patient was admitted with resting angina. The echocardiogram (Figure A) and the computed tomography-angio showed that the aneurysm had increased to 80 mm and compressed the LMCA (Figure B). This finding was confirmed on coronary angiography and intravascular ultrasound that showed a critical stenosis of LMCA (Figure C, insert 1, and online-only Data Supplement Movie I) and normal luminal diameter of anterior descending artery (Figure C, insert 2). In addition, the mean pulmonary artery pressure had increased >60 mm Hg. ...
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#左主干#
22
#JACC#
22
#ACC#
32