Nature:共生细菌产生可以模拟人信号分子的GPCR配体
2017-08-31 海北 MedSci原创
共生细菌在人类健康中起着至关重要的作用。但是至今为止,我们对它们影响哺乳动物生理特征的机制依旧知之甚少。但是毋庸置疑的是,细菌代谢物是其和宿主相互作用中的关键组成部分。 来自洛克菲勒大学的研究人员利用生物信息学和合成生物学的手段,在人类微生物群中寻找和G-蛋白偶联受体(GPCR)相互作用的N-酰基酰胺。
共生细菌在人类健康中起着至关重要的作用。但是至今为止,我们对它们影响哺乳动物生理特征的机制依旧知之甚少。但是毋庸置疑的是,细菌代谢物是其和宿主相互作用中的关键组成部分。
来自洛克菲勒大学的研究人员利用生物信息学和合成生物学的手段,在人类微生物群中寻找和G-蛋白偶联受体(GPCR)相互作用的N-酰基酰胺。
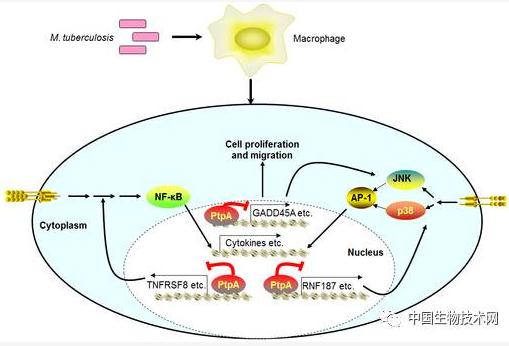
研究人员发现,肠道微生物中富含N-酰基酰胺合成酶基因,它们编码的脂质可以和GPCR相互作用,以调节胃肠道生理学特征。研究人员在小鼠和细胞模型中的研究显示,和人源配体类似,共生GPR119激动剂能够有效调节代谢激素和葡萄糖的体内平衡。但是研究人员也坦言,我们还需要未来的研究,来确定其在人类中潜在的生理作用。
因此,研究人员的结果显示,对真核生物信号分子的化学模拟在共生细菌中可能是常见的。我们可能可以通过小分子影响微生物基因编码的代谢物,改变宿主细胞应答。这是一种潜在的治疗模式(微生物生物合成基因治疗)。
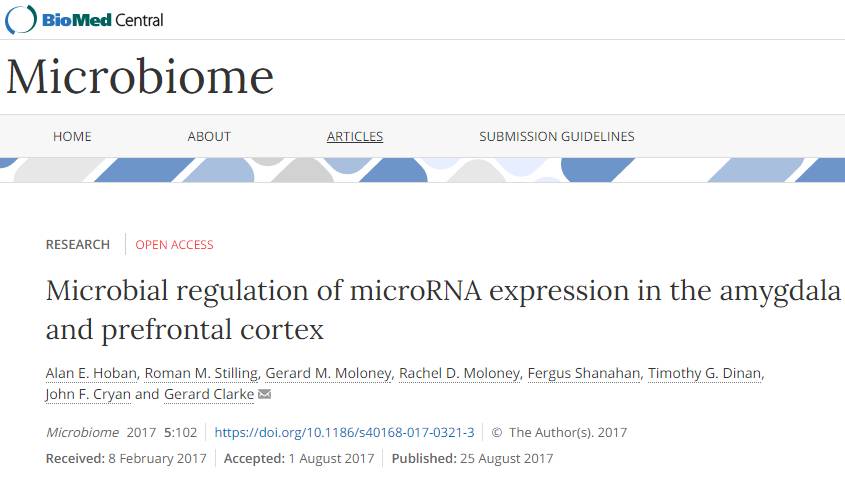
原始出处:
Louis J. Cohen et al. Commensal bacteria make GPCR ligands that mimic human signalling molecules. Nature, 2017; DOI: 10.1038/nature23874
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GPCR#
43
#PCR#
38
#Nat#
32
学习了新知识
0
期待深入研究结果
70