Advanced Materials:华人学者开发智能胰岛素降糖系统
2017-05-09 生物谷 生物谷
来自美国北卡罗来纳州立大学和北卡罗来纳大学教堂山分校的研究人员开发了一种新技术,他们通过对胰岛素进行修饰再结合红细胞构建了一个可以进行葡萄糖响应的智能胰岛素运输系统。在动物模型研究中,这种新技术能够有效降低1型糖尿病小鼠的血糖。研究人员通过化学方法将葡糖胺与胰岛素连接在一起对胰岛素进行了化学修饰。葡糖胺可以与红细胞表面的葡萄糖转运蛋白进行结合

来自美国北卡罗来纳州立大学和北卡罗来纳大学教堂山分校的研究人员开发了一种新技术,他们通过对胰岛素进行修饰再结合红细胞构建了一个可以进行葡萄糖响应的智能胰岛素运输系统。在动物模型研究中,这种新技术能够有效降低1型糖尿病小鼠的血糖。
研究人员通过化学方法将葡糖胺与胰岛素连接在一起对胰岛素进行了化学修饰。葡糖胺可以与红细胞表面的葡萄糖转运蛋白进行结合,使胰岛素能够附着在红细胞表面。这样就可以获得运载着胰岛素的红细胞。
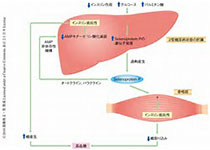
在这项研究中,研究人员将运载胰岛素的红细胞注射到1型糖尿病小鼠模型体内。一旦进入血液,携带胰岛素的红细胞就可以与环境发生作用,如果葡萄糖水平很高,葡萄糖分子就可以有效替换结合在红细胞表面葡萄糖转运分子上的葡糖胺,进而使胰岛素得到释放。胰岛素可以与肝脏、肌肉和脂肪组织的胰岛素受体结合,触发降糖过程。
研究人员共设置了三组小鼠:第一组注射生理盐水;第二组注射修饰胰岛素;第三组注射未经修饰的胰岛素和红细胞。研究人员发现接受修饰胰岛素注射的1型糖尿病小鼠能够在超过两天时间里显著降低血糖水平,而另外两组中最好的血糖控制情况也会在12小时候回到高血糖水平。
研究人员还在健康小鼠体内检测了这些药物组合,发现修饰胰岛素和血细胞运输系统能够降低低血糖症风险。除此之外,他们还利用修饰胰岛素和包裹了红细胞膜的纳米颗粒在1型糖尿病小鼠上进行了实验,发现也可以得到类似的效果。
研究人员表示,在应用于临床之前他们还会继续在动物模型上对修饰胰岛素系统进行长期评估。如果该方法能够得到应用,将会是糖尿病治疗方面取得的重要进步。
相关研究结果发表在国际学术期刊Advanced Materials上,文章通讯作者是华人学者顾臻。
原始出处:
Chao Wang,et al. Red Blood Cells for Glucose-Responsive Insulin Delivery. Advanced Marerials, DOI: 10.1002/adma.201606617
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Advanced#
45
#胰岛#
37
#华人#
29
#华人学者#
42