PLoS One:马拉维乡村地区儿科慢性化脓性中耳炎和听力损伤流行度分析
2017-12-26 AlexYang MedSci原创
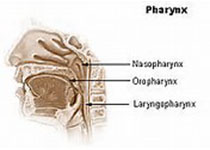
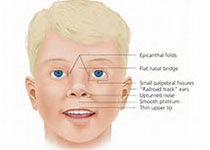
最近,有研究人员在马拉维乡村地区学龄儿童的一个群体代表性样本中,评估了世界卫生组织定义的慢性化脓性中耳炎(CSOM)和轻度听力损伤的流行,并且还探索了在该群体中与CSOM相关的因素。研究人员在马拉维Chikhwawa地区进行了与I个基于群体的代表性研究,参与研究的儿童年龄在4-6岁,并利用了一个村级水平集群设计。参与者经历了一个结构化的临床评估,包括视频耳镜检查和听觉筛选。诊断有2名耳鼻喉科专家进
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#听力损伤#
38
#流行度#
37
#化脓性#
32
#Plos one#
29
#听力#
26
#中耳炎#
29
#损伤#
26