Asian Pac J Allergy Immunol:蒸汽吸入法对过敏性鼻炎患者鼻塞影响研究
2019-06-23 AlexYang MedSci原创
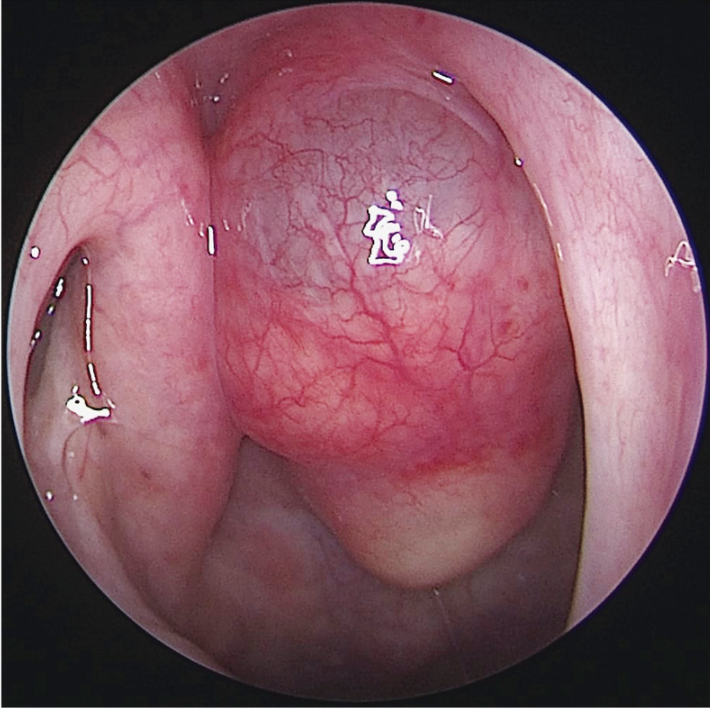
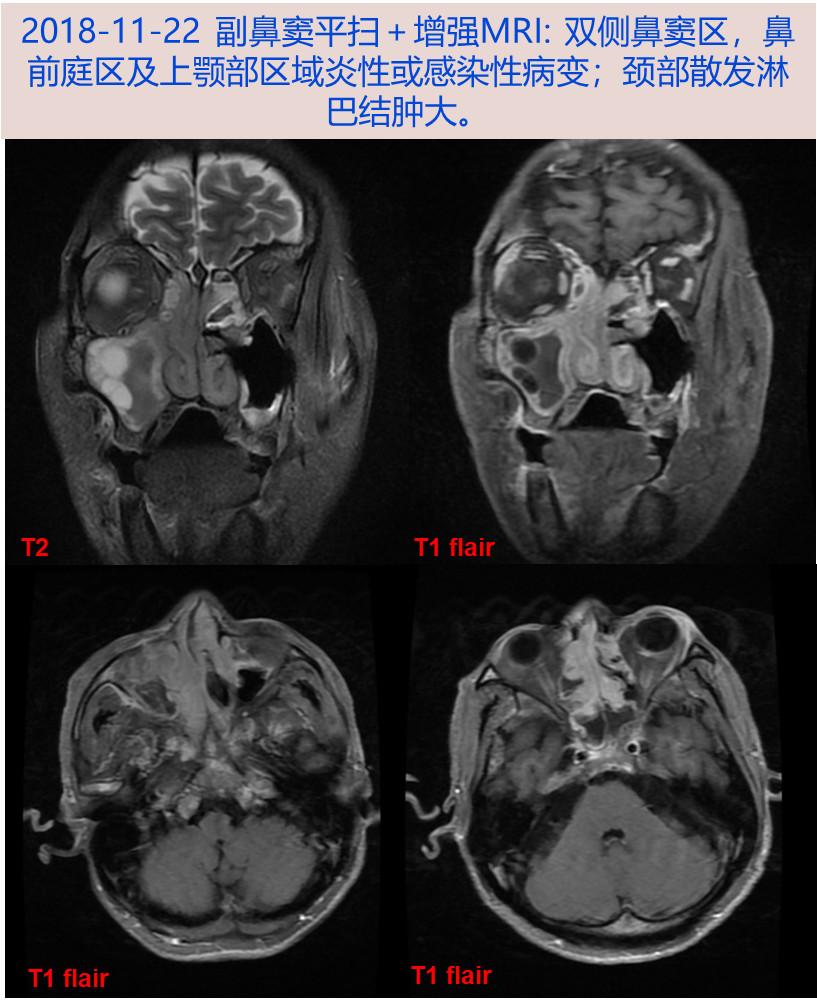
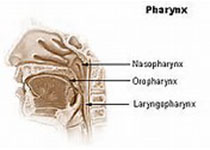
鼻塞对过敏性鼻炎(AR)患者的生活质量具有一定的影响。蒸汽吸入法是家庭中广泛应用于舒缓和打开鼻道的方法之一。更多的是,蒸汽吸入法可能为客观的气道评估带来影响。最近, 有研究人员比较了蒸汽吸入法对AR患者和正常个体鼻塞的影响,以及比较了2个小组中鼻腔横截面积和鼻气道阻力(NAR)情况。研究是一个前瞻性的、比较的和平行的研究。研究发现,蒸汽吸入法后,AR患者的鼻症状评分、综合全身症状和综合全身症状视觉
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASIA#
30
#蒸汽吸入#
31
#Asian#
30
#过敏性#
27
#ALL#
24
#鼻塞#
32