Stroke:缺血性脑卒中,静脉溶栓联合血栓切除优于单独静脉溶栓治疗
2016-06-02 phylis 译 MedSci原创
背景:缺血性脑卒中患者的随机试验表明,与药物治疗相比(包括静脉溶栓),应用新一代的取栓装置的血管内治疗有更好的功能预后。然而,在常规临床实践中患者的死亡率及预后的普遍性尚不清楚。方法:在一项前瞻性观察性研究中,研究对象为进行静脉溶栓、取栓或联合治疗的缺血性脑卒中患者。主要预后是3个月改良Rankin量表评分(0 [无症状] -6 [死亡]分)在。采用有序逻辑回归法估计治疗效果(位移分析)的一般OR
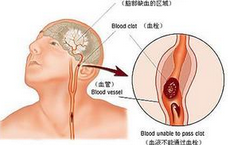
背景:缺血性脑卒中患者的随机试验表明,与药物治疗相比(包括静脉溶栓),应用新一代的取栓装置的血管内治疗有更好的功能预后。然而,在常规临床实践中患者的死亡率及预后的普遍性尚不清楚。
方法:在一项前瞻性观察性研究中,研究对象为进行静脉溶栓、取栓或联合治疗的缺血性脑卒中患者。主要预后是3个月改良Rankin量表评分(0 [无症状] -6 [死亡]分)在。采用有序逻辑回归法估计治疗效果(位移分析)的一般OR值。应用倾向评分匹配比较单独静脉溶栓治疗的和静脉溶栓联合血栓切除术治疗。
结果:2650名患者中,1543例接受静脉溶栓,504例血栓切除术,603例静脉溶栓联合血栓切除术。在手术取栓联合溶栓治疗的患者中,症状开始到治疗时间与不良预后相关。倾向评分匹配241对颅内近端闭塞患者,发现静脉溶栓联合血栓切除术与预后改善相关(常见的OR,1.84;95%CI,1.32-2.57),并且与单独静脉溶栓相比,死亡率降低(15% vs 33%)。因漏失的结果进行的敏感性分析和其他不同的分析发现显示,最后的结果是相似的。
结论:这项大型前瞻性研究结果显示,在常规临床治疗中,与单独静脉溶栓治疗相比,静脉溶栓联合血栓切除治疗改善缺血性卒中患者的功能预后,并降低其死亡率。早期治疗,预后更好。
原始出处:
Minnerup J, Wersching H,et al. Outcome After Thrombectomy and Intravenous Thrombolysis in Patients With Acute Ischemic Stroke: A Prospective Observational Study. Stroke. 2016 Jun
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
32
#缺血性#
32
#缺血性脑#
25
赞了,认真探究、学习。
64
#血栓切除#
34
#溶栓治疗#
24
#静脉溶栓治疗#
31
血栓切除可能会应用越来越广泛,他在很多研究中都证明,是有效的
104