中国自主研发冠脉药物洗脱支架美国完成第一例植入
2017-10-23 佚名 中国医学论坛报
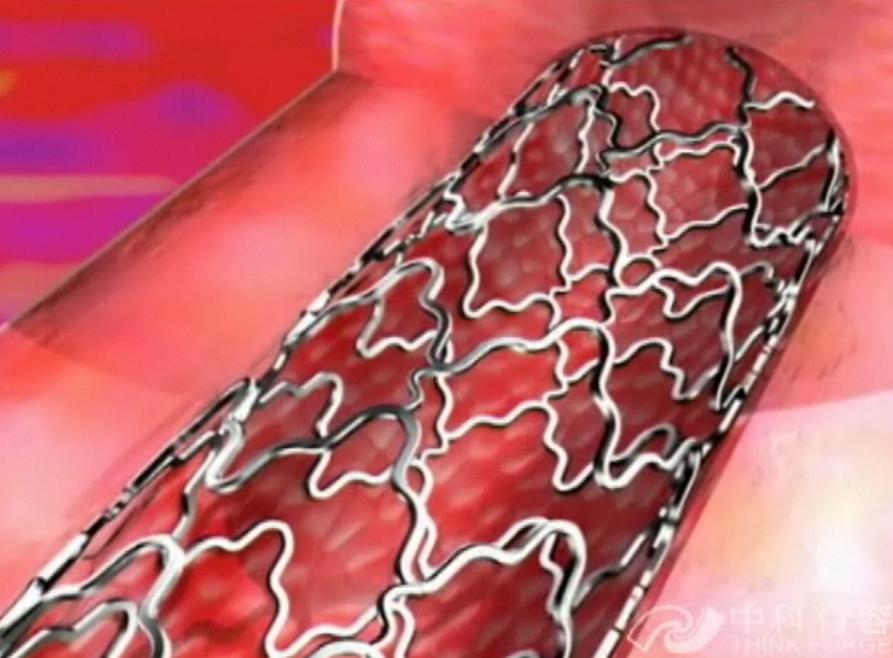
医疗器械,特别是冠脉支架,欧美原创、中国仿制的局面正在改变。旨在解决冠脉药物支架植入患者需要长期服用抗血小板药物等世界难题,由我国赛诺医疗自主研发、拥有完整知识产权,包括产品设计及特殊工艺(Know How)的冠脉药物洗脱支架在各国著名心脏介入专家领导下,自2015年开始启动了全球范围内(包括中国及欧美日等发达地区)产品注册及循证医学研究的征程。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#洗脱支架#
28
#自主研发#
36
学习一下很不错
75
学习一下很不错
75
#研发#
34
#药物洗脱支架#
38
#植入#
32
产权明晰.厉害
68