Blood:微调FOXO3A,是cHL的一种生存机制,也是流产性浆细胞分化的标志
2018-02-14 MedSci MedSci原创
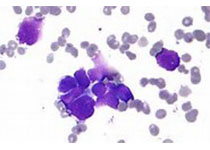
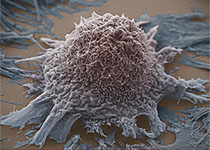
中心点:FOXO3A表达提示cHL的流产性PC分化状态。严格调控FOXO3A的表达,与cHL的病程发展至关重要。摘要:近期有研究人员发现抑制FOXO1可促进经典霍奇金淋巴瘤(cHL)的病程发展。有趣的是,另报道发现FOXO3A,FOXO家族的另一个成员,在cHL的恶性HRS细胞中的表达水平明显高于在非霍奇金淋巴瘤(NHL)亚型的表达水平。因此,研究人员对FOXO3A在cHL的潜在作用及维持其水平的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#cHL#
51
#FOXO3a#
0
#浆细胞#
59
#细胞分化#
33
学习了.谢谢作者分享!
45
关注
51