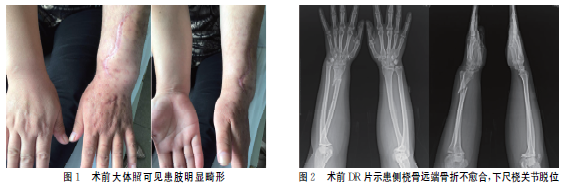
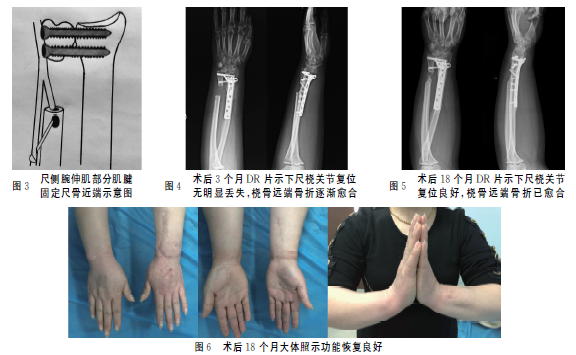
改良Sauve-Kapandji手术治疗陈旧性下尺桡关节脱位1例
2020-01-15 房燚 赵文志 潘德悦 实用骨科杂志
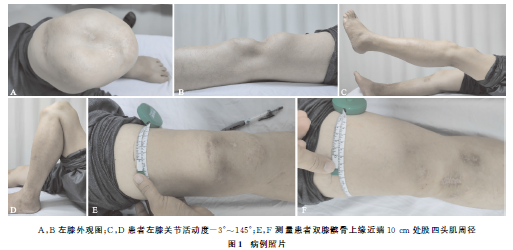
下尺桡关节脱位常发生于桡骨和/或尺骨骨折,单纯脱位或半脱位较难诊断,最初可漏诊高达50%。2017年9月我院收治1例桡骨远端骨折术后骨不连合并陈旧性下尺桡关节脱位患者,采用改良Sauve-Kapandji手术治疗,取得满意疗效,现报道如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#桡关节#
43
#关节脱位#
43
#手术治疗#
39
#APA#
38
#陈旧性#
38
#脱位#
42