NEJM:冠状动脉痉挛-案例报道
2017-06-22 xing.T MedSci原创
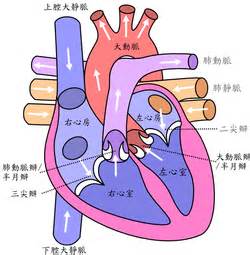
冠状动脉痉挛是以休息期间硝酸盐敏感的心绞痛发作为特征,短暂性缺血性心电图改变,有由血管收缩剂,如乙酰胆碱,引起冠状动脉痉挛的血管造影证据。
患者为一名52岁男性,吸烟,因偶发性胸痛1月余到初级保健诊所就诊。当患者每晚休息时,胸痛会发作一次,持续15分钟,无需任何干预即可缓解。舌下含服硝酸甘油可使疼痛缓解。肌钙蛋白I检测、心电图和超声心动图检查结果均正常。进行心导管检查,结果显示在右侧冠状动脉(如图A所示)和左冠状动脉轻度非阻塞性冠状动脉狭窄。往右冠状动脉内注射乙酰胆碱可引起血管痉挛,导致右冠状动脉近端完全闭塞(图B中虚线轮廓的区域为在图A中显示的造影剂,图B中消失);血管痉挛在2分钟内消失。在痉挛期间,病人报告胸痛,心电图显示前导联导联ST段抬高和前导联对应的ST段压低。诊断为冠状动脉痉挛(以前称为变异型心绞痛)。冠状动脉痉挛是以休息期间硝酸盐敏感的心绞痛发作为特征,短暂性缺血性心电图改变,有由血管收缩剂,如乙酰胆碱,引起冠状动脉痉挛的血管造影证据。该患者被给予了口服硝苯地平的处方,并建议该患者戒烟。在2年后的随访中,病人报告坚持服药,并且接受了戒烟的建议,没有进一步的胸痛发作。原始出处:Takeshi Kondo, et al. Coronary-Artery Vasospasm.N Engl J Med 2017; h
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#痉挛#
27
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
38
很好学习了感谢
53
学习了谢谢分享
46
学习了。。。。
57
冠状动脉痉挛,学习一下知识了
39
冠状动脉痉挛致变异型心绞痛,学习了
22
学习了。。。。。。。
27