CLIN CANCER RES:转移性结直肠癌患者抗EGFR单克隆抗体获得性耐药的异质性
2017-05-26 MedSci MedSci原创
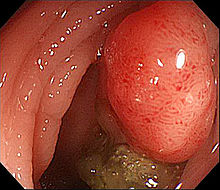
尽管RAS-BRAF野生型及HER2/MET阴性转移性结直肠癌患者通常对抗EGFR单克隆抗体有反应,但获得性耐药几乎无法避免。EGFR阻滞剂耐药的机制包括KRAS、NRAS和EGFR胞外区突变以及HER2/MET改变。但是,分子异质性如何影响患者克隆演变尚不清楚。CLIN CANCER RES近期发表了一篇文章,分析接受过抗EGFR抗体治疗的转移性结直肠癌患者肿瘤组织及血液分子特征。
尽管RAS-BRAF野生型及HER2/MET阴性转移性结直肠癌患者通常对抗EGFR单克隆抗体有反应,但获得性耐药几乎无法避免。EGFR阻滞剂耐药的机制包括KRAS、NRAS和EGFR胞外区突变以及HER2/MET改变。但是,分子异质性如何影响患者克隆演变尚不清楚。CLIN CANCER RES近期发表了一篇文章,分析接受过抗EGFR抗体治疗的转移性结直肠癌患者肿瘤组织及血液分子特征。
共有22例初始反应后接受抗EGFR治疗的RAS-BRAF野生型,HER2/MET阴性转移性结直肠癌患者再次接受活检。使用二代次序及SISH/IHC分析原始肿瘤标本及再进展肿瘤标本。收集与肿瘤组织相匹配的血标本,分析其中的循环肿瘤分子(ctDNA)。在肿瘤组织及血液标本中的分析表明RAS突变及HER2/MET扩增是最常见的耐药机制。此外,BRAF及EGFR胞外区突变相对少见。获得性MET扩增的患者接受抗EGFR治疗PFS更差。肿瘤组织及血液ctDNA共同分析结果证实了EGFR阻滞所引发的克隆演变的复杂性。
文章最后认为,转移性结直肠癌患者接受靶向治疗后出现获得性耐药的分子异质性很复杂,靶向这种复杂的分子异质性难度很大。
原始出处:
Filippo Pietrantonio,Claudio Vernieri,et
al.Heterogeneity of Acquired Resistance to Anti-EGFR Monoclonal Antibodies in
Patients with Metastatic Colorectal Cancer.CLIN CANCER RES.May 2017
doi:10.1158/1078-0432.CCR-16-1863
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#克隆#
40
#获得性#
28
#获得性耐药#
44
#转移性#
32
#结直肠#
28
#GFR#
35
应该重视学习。
60
受教了,感谢分享
47
好东西学习了!
70
谢谢分享,学习了很多有用的知识!
58