JAMA:高灵敏度cTnT与二级预防的心血管事件相关
2013-04-17 Jama dxy
最新研究表明,稳定性冠脉心脏病门诊患者的高敏心肌肌钙蛋白T(hs-cTnT)水平与继发性心血管事件风险升高呈独立相关性。 Alexis Beatty博士(旧金山加州大学)和他的同事发表在2013年4月8日的《JAMA:内科学》上)研究表明,hs-cTnT水平可对不能被现有心血管疾病严重程度指标衡量的风险因素进行量化。数据来自
最新研究表明,稳定性冠脉心脏病门诊患者的高敏心肌肌钙蛋白T(hs-cTnT)水平与继发性心血管事件风险升高呈独立相关性。
Alexis Beatty博士(旧金山加州大学)和他的同事发表在2013年4月8日的《JAMA:内科学》上)研究表明,hs-cTnT水平可对不能被现有心血管疾病严重程度指标衡量的风险因素进行量化。
数据来自一项前瞻性队列研究,这项研究旨在评估社会心理因素对稳定型冠状动脉心脏疾病患者临床预后的影响。从2000年到2002年,共有来自12家门诊的984例患者入选,研究人员测量了血清hs-cTnT 水平并进行了平板运动负荷超声心动图检测。对患者随访8.2年(中位数),在此期间,133例患者患心肌梗死,180例曾因心脏衰竭到医院就诊,146人死于心血管疾病(317例患者出现心血管死亡、心脏衰竭住院,或心肌梗死)。
共有794例(80.7%)受试者基线时检出(定义为> 5 pg/ml)。相比之下,采用标准检测法,只有58名受试者检出hs-cTnT检测肌钙蛋白。hs-cTnT水平较高明显与缺血更重,左心室射血分数,左心房功能,舒张功能,左室质量,和平板运动能力更差相关。
使用hs-cTnT水平进行分层,中等hs-cTnT水平(7.12-13.67 pg/mL)个体的心血管事件风险比低hs-cTnT水平(<7.09 pg/mL)个体高75%。与最低水平个体相比,最高hs-cTnT组(> 13.67 pg/mL)患者的MI,心脏衰竭住院或心血管死亡风险增加五倍多。
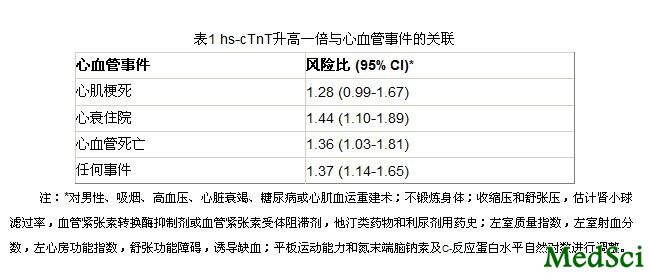
在本组患者中,hs-cTnT升高可能与心脏疾病的结构和功能指标有关,但即使调整这些指标后,hs-cTnT每增加一倍仍引起心血管事件风险增加37%。
在这篇文章中,研究人员对hs-cTnT水平与稳定型冠状动脉心脏疾病患者继发心血管事件之间的关联进行了评估。这些分析表明,高灵敏度检测法检测的肌钙蛋白水平与未来的心血管事件有关,且有助于提高风险预测。
据Beatty 等人称,他们的研究证实了这些发现并将其延伸至以下三个方面:1)他们已经发现,一般冠状动脉心脏疾病门诊就诊人群中超过3/4的患者可检出hs-cTnT。2)他们已经发现,hs-cTnT水平与心脏结构和功能异常有关。3)他们已经证实,即使对心脏疾病严重程度指标进行调整后,hs-cTnT水平仍与目前稳定性冠心病患者的继发心血管事件相关。“
能改善风险分层,但它会改变现有的护理?
《JAMA:内科学编辑》Patrick O'Malley博士(华盛顿沃尔特•里德陆军医疗中心)指出,研究结果表明有能力进一步完善稳定型冠状动脉心脏疾病患者的风险预测,虽然是否应该去做是另外一个问题。他指出,目前尚不清楚这些信息将如何改变已经治疗的患者
那些低肌钙蛋白水平的患者仍然有20%的10年心血管事件风险,所以新的信息不会改变他们的用药。对于高肌钙蛋白水平患者,医生可以考虑对预后进行更细致的讨论或考虑进行二级预防试验来评估新的治疗方法。
与心血管相关的拓展阅读:
- 心血管领域临床进展及SCI论文和基金写作-MedSci快报(第72期)
- Sirtuins---在心血管系统的作用全面解析
- Diabetes Care:低血糖症增加心血管事件风险
- Nat Rev Cardiol:戒烟降低非糖尿病患者心血管疾病风险
- Am Heart J:高甲状旁腺激素水平增加心血管病事件风险
- JAMA Intern.Med:补钙提高男性心血管疾病死亡率
- 更多信息请点击:有关心血管更多资讯

High-Sensitivity Cardiac Troponin T Levels and Secondary Events in Outpatients With Coronary Heart Disease From the Heart and Soul Study.
IMPORTANCE
Levels of high-sensitivity cardiac troponin T (hs-cTnT) predict secondary cardiovascular events in patients with stable coronary heart disease.
OBJECTIVES
To determine the association of hs-cTnT levels with structural and functional measures of heart disease and the extent to which these measures explain the relationship between hs-cTnT and secondary events. DESIGN We measured serum concentrations of hs-cTnT and performed exercise treadmill testing with stress echocardiography in a prospective cohort study of outpatients with coronary heart disease who were enrolled from September 11, 2000, through December 20, 2002, and followed up for a median of 8.2 years. SETTING Twelve outpatient clinics in the San Francisco Bay Area.
PARTICIPANTS
Nine hundred eighty-four patients with stable coronary heart disease.
MAIN OUTCOMES AND MEASURES
Cardiovascular events (myocardial infarction, heart failure, or cardiovascular death), determined by review of medical records and death certificates.
RESULTS
Of 984 participants, 794 (80.7%) had detectable hs-cTnT levels. At baseline, higher hs-cTnT levels were associated with greater inducible ischemia and worse left ventricular ejection fraction, left atrial function, diastolic function, left ventricular mass, and treadmill exercise capacity. During follow-up, 317 participants (32.2%) experienced a cardiovascular event. After adjustment for clinical risk factors, baseline cardiac structure and function, and other biomarkers (N-terminal portion of the prohormone of brain-type natriuretic peptide and C-reactive protein levels), each doubling in hs-cTnT level remained associated with a 37% higher rate of cardiovascular events (hazard ratio, 1.37 [95% CI, 1.14-1.65]; P = .001).
CONCLUSIONS AND RELEVANCE
In outpatients with stable coronary heart disease, higher hs-cTnT levels were associated with multiple abnormalities of cardiac structure and function but remained independently predictive of secondary events. These findings suggest that hs-cTnT levels may detect an element of risk that is not captured by existing measures of cardiac disease severity.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#cTnT#
28
#灵敏度#
44
#血管事件#
24