本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2017-08-13 Pumch-EM 急诊界
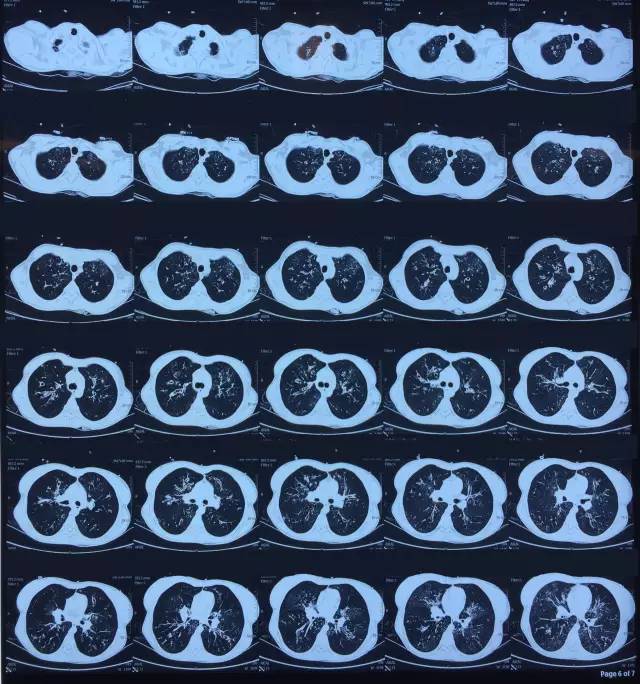
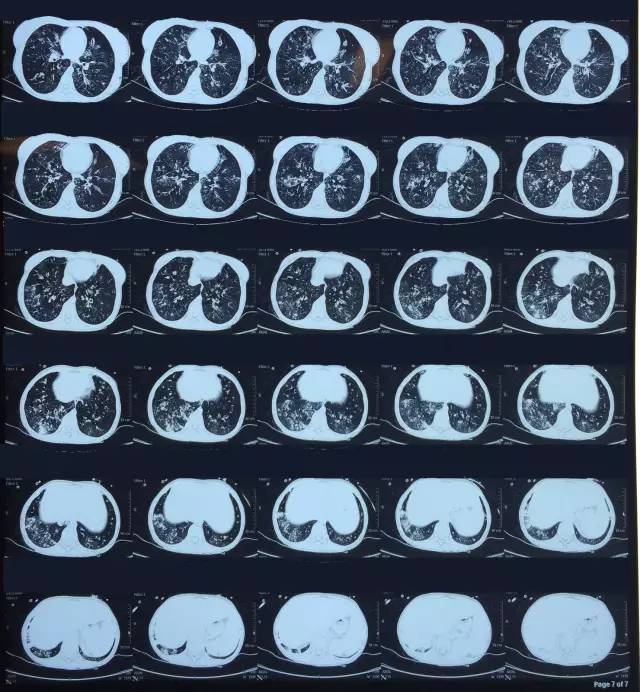
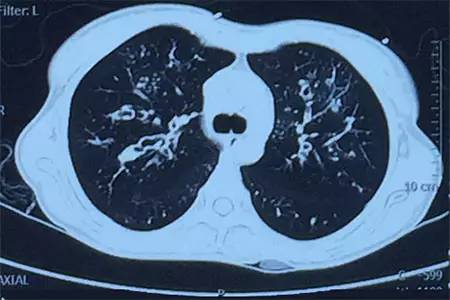
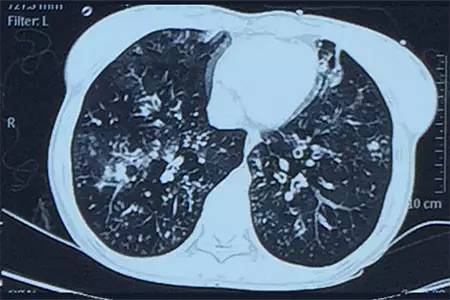
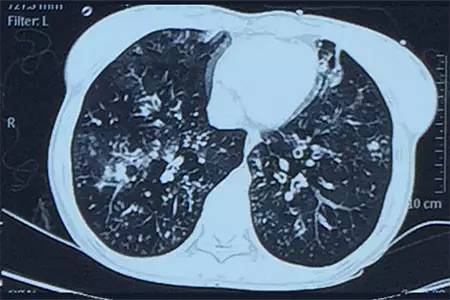
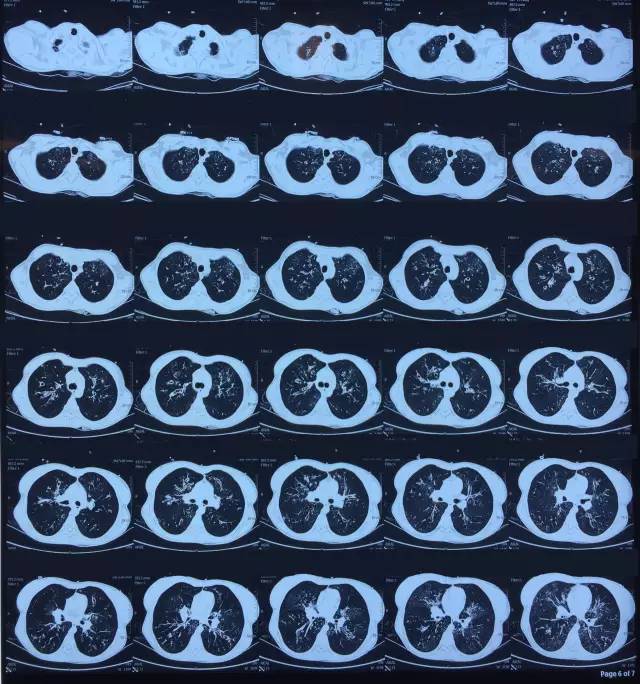
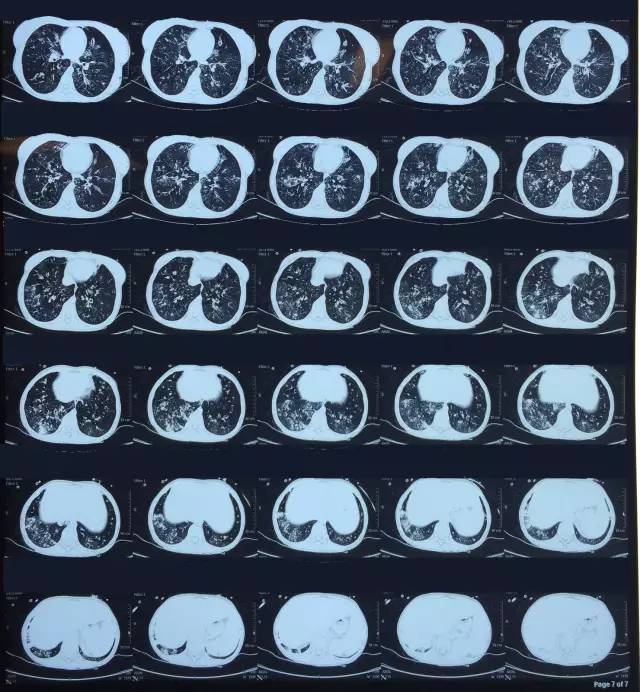
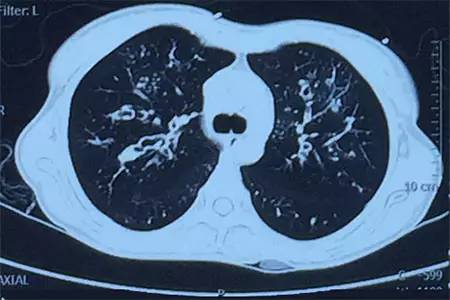
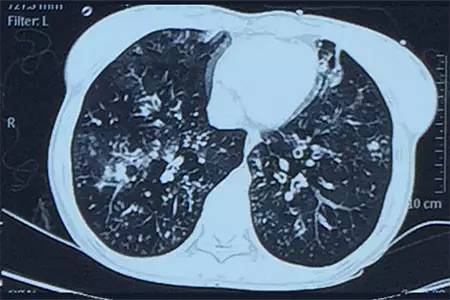
病例:患者女性,21岁,间断咳嗽、咳痰3年,加重伴发热10日。

在两个支气管扩张患者的全国性的样本中ICS的使用是很常见的,相对较少的患者接受了抑制性抗生素治疗。需要进一步的研究以明确这些疗法在支气管扩张症患者的安全性和有效性。
两个为期一年的随机临床试验证实,红霉素和阿奇霉素这两个大环内酯类抗生素可减轻非囊性纤维化支气管扩张肺感染的急性加剧,但代价是对这两个药的抗药性增加。据澳大利亚南布里斯班Mater成人医院的David Serisier (MBBS,DM)及其同事所说,在BLESS临床试验中,每日低剂量红霉素维持治疗的患者,其肺感染急性加剧率明显低于使用安慰剂的患者(1.29 vs 1.97人年,发病率比0.57,9
对于非囊性纤维化(CF)支气管扩张成人患者而言,感染在疾病进展中发挥着潜在的重要作用。尽管感染在成人非囊性纤维化(CF)支气管扩张疾病进展中有潜在的重要作用,然而对于这些患者下呼吸道的菌群特点的描述却很少。针对这种情况,来自伦敦大学国王学院医药科学研究所的Kenneth Bruce博士等人进行了一项研究,研究结果在线发表于2013年4月6日的《胸部》(Thorax)杂志上。作者发现非CF支气管扩张
由此可见,该研究结果表明阿托伐他汀可以降低感染铜绿假单胞菌的支气管扩张患者全身炎症和改善生活质量。这些效应可能是由于阿托伐他汀调节中性粒细胞活化能力所致。
目的:针对支气管扩张患者和没有肺疾病的受试者,分析他们的黏液性和化脓性呼吸道分泌物的情况。 方法:在咳嗽模拟器中,他们评估粘液纤毛传送功能在支气管扩张症中的作用,共收集了32个黏液性标本和19个化脓性标本以及没有肺疾病受试者的21个标本。 结果:化脓性标本和黏液性标本粘液纤毛传送功能较没有肺疾病患者的标本低。在咳嗽模拟器中化脓性标本相比粘液性标本和没有肺疾病患者的标本更不容易移动,粘液


梅斯医学MedSci APP
医路相伴,成就大医
#支气管#
39
#扩张#
31
学习谢谢分享
79
学习,谢谢分享
78