JACC子刊:冠状动脉钙化会增加癌症、慢性肾脏病、COPD和骨折的风险!
2016-03-25 Seven L 译 MedSci原创
研究者进行了一项研究,探究冠状动脉钙化(CAC)与非心血管疾病风险间的联系。该研究纳入了6814名参与者,中位数随访10.2年。校正年龄、性别、种族,社会经济地位、健康保险状态、BMI、运动、饮食、吸烟、使用的药物情况、收缩压、舒张压、总胆固醇、高密度脂蛋白胆固醇、抗高血压、阿司匹林、胆固醇药物和糖尿病等混杂因素,使用改良后的Cox比例风险模型计算了致命性冠心病对新诊断的癌症、肺炎、慢性阻塞性肺疾
研究者进行了一项研究,探究冠状动脉钙化(CAC)与非心血管疾病风险间的联系。
该研究纳入了6814名参与者,中位数随访10.2年。校正年龄、性别、种族、社会经济地位、健康保险状态、BMI、运动、饮食、吸烟、使用的药物情况、收缩压、舒张压、总胆固醇、高密度脂蛋白胆固醇、抗高血压药、阿司匹林、胆固醇药物和糖尿病等混杂因素,使用改良后的Cox比例风险模型计算了致命性冠心病对新诊断的癌症、肺炎、慢性阻塞性肺疾病(COPD)、慢性肾脏疾病(CKD)、深静脉血栓形成/肺栓塞、髋部骨折和痴呆的风险。以新诊断的非心血管疾病作为结局指标。
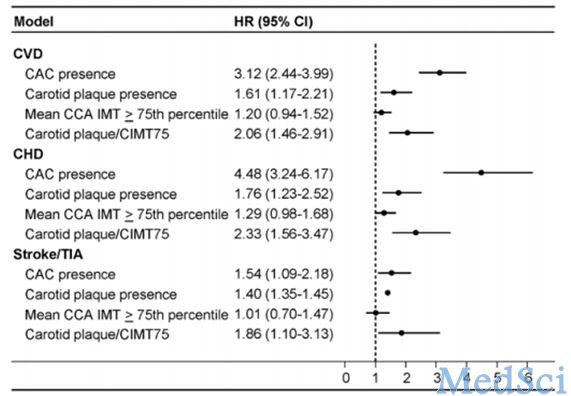
研究数据显示,与CAC = 0的参与者相比,CAC >400的参与者其癌症 (HR: 1.97; 95% CI: 1.37 to 2.82)、CKD (HR: 1.70; 95% CI: 1.21 to 2.39)、肺炎(HR: 1.97; 95% CI: 1.37 to 2.82)、COPD(HR: 2.71; 95% CI: 1.60 to 4.57)和髋部骨折(HR: 4.29; 95% CI: 1.47 to 12.50)风险均增加。不过深静脉血栓形成/肺栓塞和痴呆的风险没有增加。
相反,与CAC>0的参与者相比,CAC=0的参与者的癌症(HR: 0.76; 95% CI: 0.63 to 0.92)、CKD(HR: 0.77; 95% CI: 0.60 to 0.98)、COPD(HR: 0.61; 95% CI: 0.40 to 0.91)和髋部骨折(HR: 0.31; 95% CI: 0.14 to 0.70)风险下降。不过CAC=0并不意味者肺炎、痴呆和深静脉血栓形成/肺栓塞风险的下降。
虽然在排除掉临时非致命性冠心病患者后,这些风险间的联系有所衰减,但是仍具有统计学意义。
研究结果表明,随着CAC的增高,参与者癌症、CKD、COPD和髋部骨折风险增加。而CAC=0的参与者患上与年龄相关的并发症的风险更低,这代表了一类独特的人群“健康时代的人”。
原始出处:
Handy CE,Desai CS,Dardari ZA,Al-Mallah MH,et al.The Association of Coronary Artery Calcium With Noncardiovascular Disease: The Multi-Ethnic Study of Atherosclerosis.JACC Cardiovasc Imaging 2016 Mar 3;[Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠状动脉钙#
28
#动脉钙化#
30
#JACC#
38
希望有更深入的研究
77
#冠状动脉钙化#
28
#ACC#
26
#慢性肾脏#
21
随访时间长,样本量大,学习了
112