日本批准CABOMETYX(cabozantinib)治疗无法切除的或转移性肾细胞癌
2020-03-25 Allan MedSci原创
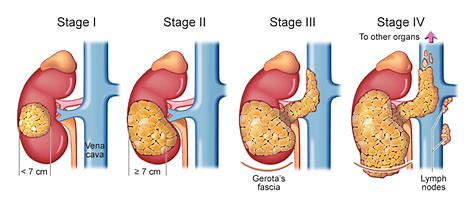
Exelixis制药公司今日宣布,CABOMETYX®(cabozantinib)已获得日本厚生劳动省的批准,用以治疗无法切除的或转移性肾细胞癌(RCC)患者。
Exelixis制药公司今日宣布,CABOMETYX®(cabozantinib)已获得日本厚生劳动省的批准,用以治疗无法切除的或转移性肾细胞癌(RCC)患者。该批准基于以下三项临床试验:(1)METEOR研究,cabozantinib vs. everolimus治疗先前接受过至少一种VEGF受体酪氨酸激酶抑制剂(VEGFR-TKI)治疗的RCC患者;(2)CABOSUN研究,cabozantinib vs. sunitinib治疗初治中度或低危疾病晚期RCC患者;(3)Cabozantinib-2001研究。
Exelixis总裁Michael M. Morrissey博士说:“据估计,日本每年新增约17,000例肾细胞癌病例,由于许多病例被诊断为晚期,因此这些患者的预后仍然很差。CABOMETYX的批准对于日本的肾癌患者来说是一个重要的里程碑”。
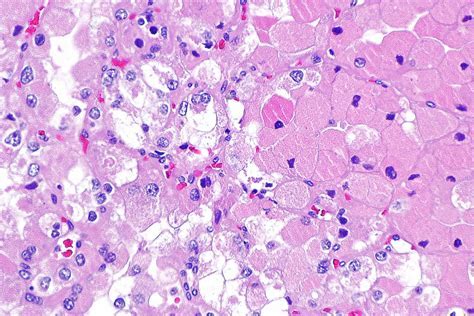
CABOMETYX®(cabozantinib)早在2012年11月29日就经美国FDA批准用于不可手术切除的恶性局部晚期或转移性甲状腺髓样癌。cabozantinib能够抑制多种激酶受体,包括RET、MET、VEGFR-1、VEGFR-2、VEGFR-3、KIT、TRKB,以上激酶受体在正常细胞和肿瘤细胞生长过程中均起着重要作用。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#MET#
22
#细胞癌#
21
#日本#
28
#转移性#
33
#转移性肾细胞癌#
38
#cabozantinib#
38
#ABO#
22