Blood:抗磷脂抗体通过内皮细胞中形成的apoER2-Dab2-SHC1复合体激活PP2A诱导血栓形成
2018-03-04 MedSci MedSci原创
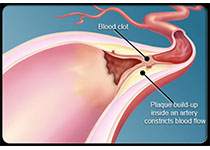
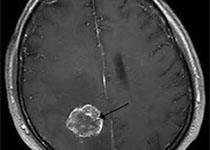
中心点:激活内皮细胞的PP2A是aPL诱导小鼠血栓形成的基础。内皮ApoER2充当aPL诱导组装的包含Dab2和SHC1的可激活PP2A的蛋白复合物的支架。摘要:对于抗磷脂抗体综合征(APS),抗磷脂抗体(aPL)识别β2糖蛋白(β2GPI)会促进血栓形成,而根据临床前研究提示,这是因为内皮NO合成酶(eNOS)通过ApoER2依赖性方式发挥拮抗作用。但其潜在的分子机制尚未明确。近日Blood上发
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复合体#
30
#抗磷脂抗体#
46
#APOE#
32
学习了.谢谢分享.
64
阅
63