中国头颈部动脉粥样硬化诊治共识:这三类人应该吃他汀
2017-10-10 卢芳 中国循环杂志
中国慢病前瞻性研究一项新的分析显示,中国有三分之一成人存在颈动脉粥样硬化斑块。对于颈动脉粥样硬化,该怎么办?
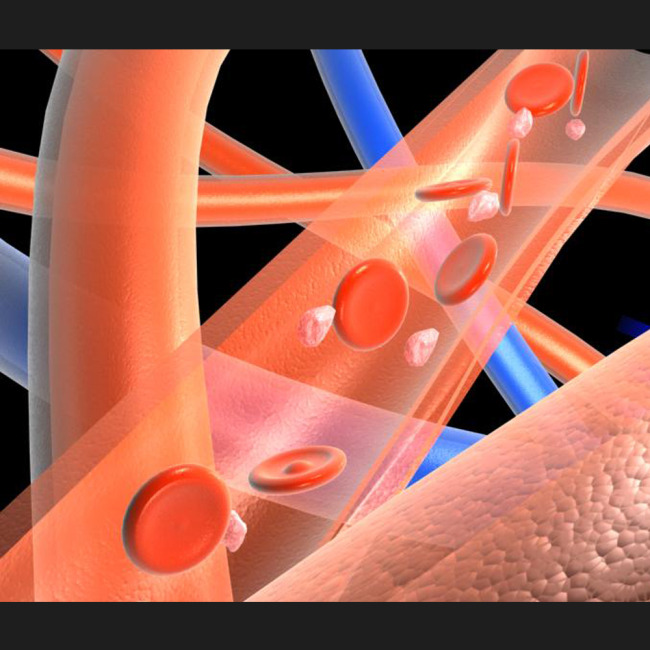
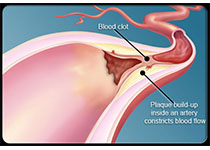
中国慢病前瞻性研究一项新的分析显示,中国有三分之一成人存在颈动脉粥样硬化斑块。对于颈动脉粥样硬化,该怎么办?近期,中华医学会神经病学分会、中华医学会神经病学分会脑血管病学组就此发布了《中国头颈部动脉粥样硬化诊治共识》。共识指出,如果一个人发生过缺血性中风,无论仅仅是有颈动脉内中膜增厚,还是仅有狭窄不严重的斑块,都建议使用他汀类药物治疗。其次,如果从形态学上判断颈动脉斑块不稳定,或者狭窄>50%,无论血脂是否异常,也都建议使用他汀类药物治疗,使LDL-C控制在1.8 mmol/L以下。如果有颈动脉斑块伴斑块狭窄,但狭窄不到50%,也没有缺血性中风,血脂也不高,可根据斑块的稳定性个体化选用他汀类药物治疗。但如果仅仅是颈动脉内中膜增厚,没有缺血性中风,就控制高血压、糖尿病、血脂异常和吸烟饮酒等相关危险因素即可。如果血脂在正常范围以内,不建议使用他汀类药物治疗。该指南也对颈内动脉剥脱术和颈动脉支架植入术也做了相应推荐。原始出处:中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组. 中国头颈部动脉粥样硬化诊治共识. 中华神经科杂志, 2017, 50: 572-578.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
37
谢谢分享.学习了
54
#头颈部#
33
#颈部#
27
你看实名认证了大家发言多么和谐
58
学习了
57