冠脉微血管功能障碍:新概念、新进展
2020-03-22 心在线 心在线
冠脉造影是诊断冠心病的一种常用且有效的方法,但它只能检测到5%的冠脉树,95%的冠脉微血管不可见。尽管冠状动脉微血管分布远较心外膜冠状动脉血管广泛,但因其结构及功能不能为常规冠脉造影技术显示,因此,冠
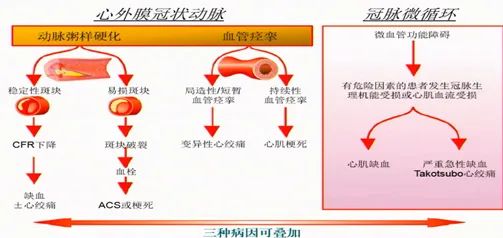
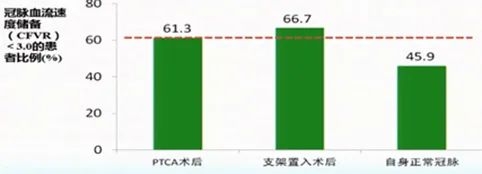
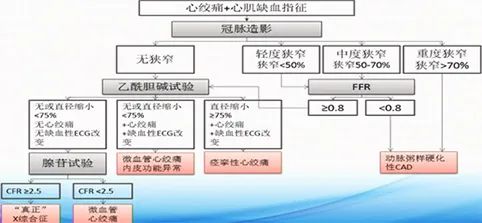
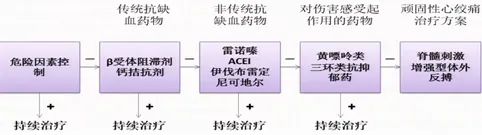
冠脉造影是诊断冠心病的一种常用且有效的方法,但它只能检测到5%的冠脉树,95%的冠脉微血管不可见。尽管冠状动脉微血管分布远较心外膜冠状动脉血管广泛,但因其结构及功能不能为常规冠脉造影技术显示,因此,冠状动脉微血管功能障碍的临床意义没有得到医生的足够重视。 一、新概念与发病机制 任何导致冠状动脉微血管功能障碍(CMD)和/或结构异常,最终都导致CMD,它是导致胸痛症状重要的病理生理学基础。CMD患者的临床表现复杂多样,建议称为冠状动脉微血管功能障碍综合征(CMDS),CMD也是冠状动脉疾病治疗的新靶点。 多部指南指出,微循环障碍在心肌缺血中发挥重要作用 1. ACC/AHA NSTE-ACS患者管理指南:冠状动脉微血管疾病和血管内皮功能障碍在非阻塞性冠心病患者的病理生理中发挥重要作用。 2. CCS 稳定性缺血性心脏病诊断和管理指南:微血管疾病会导致心肌缺血。 3. JCS 血管痉挛性心绞痛诊断和治疗指南:冠状动脉微循环异常会导致心肌缺血;冠状动脉微血管痉挛无法通过血管造影来检查,必须通过诱发试验来间接测试。 4. 2019 ESC 慢性冠脉综合征诊断和治疗指南: 冠状动脉疾病处于动态变化的过程,临床表现多种多样,可以分为急性冠脉综合征(ACS)和慢性冠脉综合征(CCS)。在目前的CCS指南中,确定了以下最常见的6种临床情况。 (1)怀疑有冠心病,有稳定的心绞痛症状和/或呼吸困难的患者; (2)新发心力衰竭或左心室功能衰竭,怀疑冠心病的患者; (3)ACS后1年内或近期血运重建的无症状或症状稳定患者; (4)初次诊断或血运重建1年以上的无症状或有症状患者; (5)心绞痛,疑似血管痉挛或微血管疾病患者; (6)筛查时发现冠心病的无症状患者。 二、心肌缺血机制的现代认识 2013年我国重新定义了稳定性冠心病(SCAD),扩大了疾病范畴,包括梗阻性+非梗阻性冠状动脉疾病(冠状动脉微血管功能 心肌缺血发病机制的示意图,如下所示。 CLINICAL研究 CLINICAL研究纳入80例心肌缺血患者,乙酰胆碱或麦角新碱激发试验阳性37例(46.2%),并无并发症;心外膜痉挛24例(64.9%),微血管痉挛13例(35.1%)。中位随访36个月显示,激发阳性试验患者的死亡率显著高于阴性患者。 CMD与阻塞性冠心病共存比例高 研究纳入212例冠脉显著狭窄(>50%)的冠心病患者,评估经皮冠状动脉腔内成形术(PTCA)或支架置入术前后的冠脉血流储备速度(CFVR)改变。CFVR≥3.0定义为正常参考值的切点。 结果显示,PTCA和支架置入术后CFVR<3.0的患者比例均超过60%,如下图所示。 冠状动脉微血管功能障碍诊断流程图,如下图所示。 2018年国际心脏病微血管性心绞痛(MVA)诊断标准 1. 心肌缺血症状 a. 静息或运动心绞痛; b. 心绞痛等危征,如气短。 2. 无阻塞性冠心病(冠脉狭窄<50%或FFR>0.8) a. CTA检查; b. 冠脉造影。 3. 心肌缺血客观证据 a. 心绞痛时心电图缺血性改变; b. 运动诱发心绞痛和/或心电图缺血性改变(无论有无心肌灌注异常),和/或室壁运动异常。 4. 冠状动脉微血管功能受损的证据 a. 冠脉血流储备(CFR); b. 冠状动脉微血管痉挛; c. 微循环阻力系数(IMR); d. 冠状动脉慢血流现象。 三、检测是CMD研究瓶颈 1. 微血管功能评估的方法和指标 2. CMD检测:“先无创,后有创” 四、微血管性心绞痛治疗与研究方向 在冠状动脉微血管性心绞痛(MVA)管理方面,目前尚缺乏大型研究以及基于证据的治疗建议。冠状动脉MVA治疗流程,如下图所示。 MVA的主要管理目标 (1)改善或消除心肌缺血,纠正病因; (2)提高生活质量; (3)改善预后,识别并干预影响临床结局的因素。 五、缺血性心脏病的评价目标及治疗 1. 内皮功能障碍、可改变的心血管危险因素和生活方式管理 大多数原发性MVA和CMD患者存在内皮功能障碍,超声研究显示大部分患者存在非阻塞性冠心病。对于大多数MVA患者,应积极管理所有可改变的传统危险因素,例如高血压、糖尿病、吸烟、肥胖、久坐的生活方式、高脂血症等。 对于无阻塞性冠心病但存在冠脉内皮或血管平滑肌功能障碍的患者,他汀类药物单独使用或联合其他药物是有益的。ACEI 也被证明可以改善运动耐量和心绞痛症状。二甲双胍可改善无糖尿病的MVA患者的内皮功能。 ACC/AHA慢性稳定性心绞痛指南建议无阻塞性冠心病的心肌缺血患者使用阿司匹林,但不是强烈推荐。 2. 心肌缺血的预防和治疗 目前缺乏抗心绞痛药物治疗MVA有效的有力证据。对于有微血管痉挛或CFR异常的患者,钙通道阻滞剂可作为首选药物。 β受体阻滞剂可单独与血管扩张剂联合用于MVA患者。但微血管或心外膜血管痉挛的患者使用β受体阻滞剂应谨慎。 硝酸酯类对MVA的改善作用不明显。目前有证据表明,使用一氧化氮前体L-精氨酸可改善CMD。 尼可地尔是一种钾ATP通道开放剂,有研究显示对MVA患者有益。 法舒地尔是一种Rho激酶抑制剂和强效的冠状动脉扩张剂,可用于治疗心外膜冠状动脉痉挛,也被证明对CMD患者有效。 伊伐布雷定可以通过减慢心率而降低心肌需氧量,但目前关于这种药物对MVA患者疗效的信息很少。 一项曲美他嗪用于MVA患者的小型试点研究显示,该药可改善症状以及运动能力。 雷诺嗪是晚期钠电流抑制剂,可改善女性非阻塞性冠心病、存在CMD相关心肌缺血患者的临床症状和CFR,但也有一些研究得出阴性结果。 3. 其他治疗 有研究者提出可将三环类抗抑郁药用于MVA患者,这类药物具有镇痛作用。有研究显示,丙咪嗪可改善无阻塞性冠心病胸痛患者的症状,但副作用常见而且需停药。 黄嘌呤衍生物如氨茶碱,可通过阻断腺苷受体产生镇痛作用,改善胸痛患者的运动耐量和运动诱发的心肌缺血。 六、干预策略 1. 传统血管扩张剂:硝酸酯类、钙通道阻滞剂、硝普钠和腺苷。 2. 钾通道开放剂:尼可地尔。 3. 抗血小板药物:糖蛋白Ⅱb/Ⅲa受体拮抗剂如阿昔单抗、依替巴肽和替罗非班;ADP受体拮抗剂和阿司匹林。 4. 器械干预:血栓抽吸和远端保护装置。 5. 中医药:丹参乙酸镁盐、通心络和麝香保心丸。 参考资料 曾定尹. 冠状动脉微血管功能障碍——新概念、进展. 长城会2019.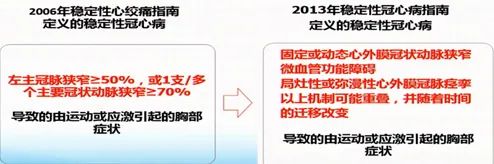


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







这个好
8
#冠脉微血管功能#
44
#微血管功能障碍#
49
#微血管#
35
#功能障碍#
31
#血管功能#
49