J Clin Oncol:化疗为手术切除的ER阴性ILRR患者带来希望
2018-06-09 张琪 环球医学网
发表在《J Clin Oncol》的CALOR试验的最终分析,考察了孤立性区域局部复发(ILRR)的雌激素受体(ER)阴性和ER阳性乳腺癌接受化疗(CT)的有效性。 目的:ILRR可预测进展乳腺癌远处转移和死亡的高风险。化疗作为局部复发乳腺癌辅助治疗(CALOR)试验考察了ILRR局部治疗后CT的有效性。中位随访5年的报告显示,CT对于ER阴性ILRR患者具有显着获益,但需要在ER阳性I
目的:ILRR可预测进展乳腺癌远处转移和死亡的高风险。化疗作为局部复发乳腺癌辅助治疗(CALOR)试验考察了ILRR局部治疗后CT的有效性。中位随访5年的报告显示,CT对于ER阴性ILRR患者具有显着获益,但需要在ER阳性ILRR患者中进行额外的随访研究。
患者和方法:CALOR是一项开放性随机试验,纳入了单侧乳腺癌后完全切除的ILRR患者。符合条件的患者被随机分配到接受CT组或未接受CT组,并根据既往CT、激素受体状态和ILRR的位置进行分层。激素受体阳性ILRR患者接受了辅助内分泌治疗。显微镜下切缘受累的患者强制放疗,抗人表皮生长因子受体2治疗非强制。终点为无疾病生存期(DFS)、总生存期和无乳腺癌间隔。
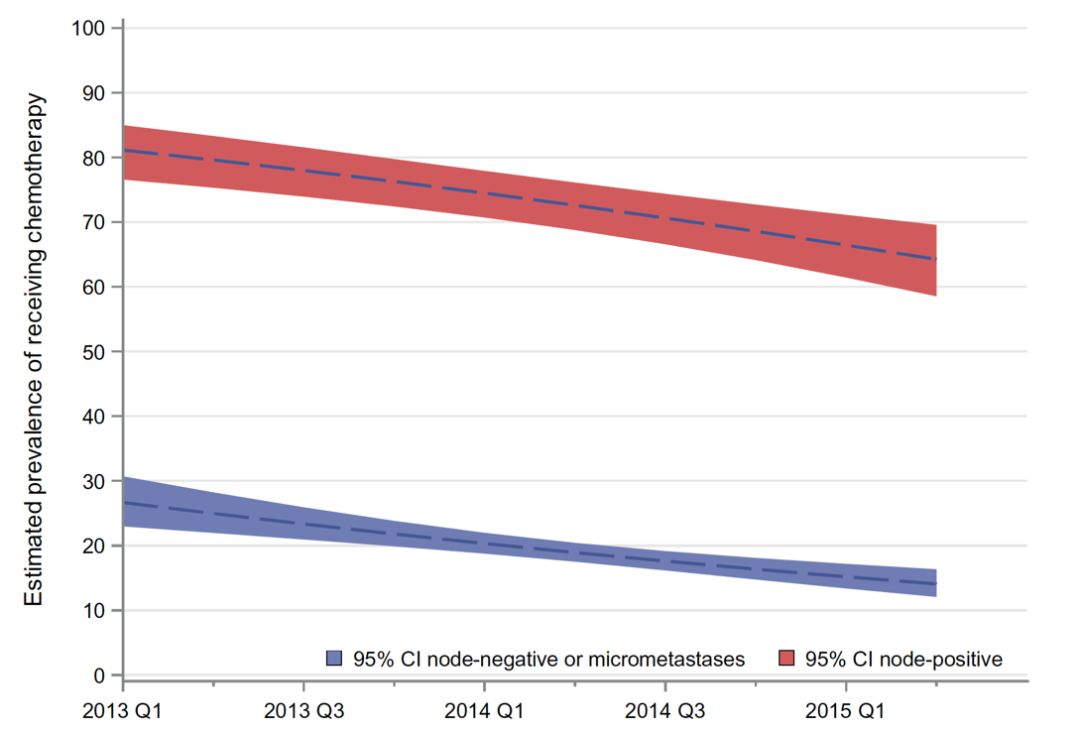
结果:2003年8月~2010年1月,纳入了162例患者:ER阴性58例,ER阳性ILRR 104例。9年的中位随访时,ER阴性组和ER阳性组分别发生27例和40例DFS事件。ER阴性ILRR患者的DFS事件风险比(HR)为0.29(95% CI,0.13~0.67;CT组和非CT组的10年DFS率分别为70% vs 34%),ER阳性ILRR患者为1.07(95% CI,0.57~2.00;10年DFS,50% vs 59%)(P=0.013)。无乳腺癌间隔的HRs分别为0.29(95% CI,0.13~0.67)和0.94(95% CI,0.47~1.85)(P=0.034),OS分别为0.48(95% CI,0.19~1.20)和0.70(95% CI,0.32~1.55)(P=0.53)。3个终点的结果在调整了ILRR位置、既往CT和原手术间隔的多变量分析中保持一致。
结论:CALOR最终分析证实,CT可使经过手术切除的ER阴性ILRR患者获益,不支持ER阳性ILRR患者使用CT。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
28
学习了受益匪浅
35
学习了受益匪浅
45
学习了.谢谢分享
3
#手术切除#
0
学习了受益匪浅
33