老年男性,右肾上腺肿物,请诊断?
2019-03-19 不详 影像园
患者1年前无明显诱因发现右肾上腺肿物,无高血压,无低钾,无发热、头晕、心悸、多汗,无腹部及腰背部疼痛,无尿频、尿急、尿痛。
【所属科室】
普外科
【基本资料】
患者,男,55岁
【主诉】
发现右肾上腺肿物1年
【现病史】
患者1年前无明显诱因发现右肾上腺肿物,无高血压,无低钾,无发热、头晕、心悸、多汗,无腹部及腰背部疼痛,无尿频、尿急、尿痛。
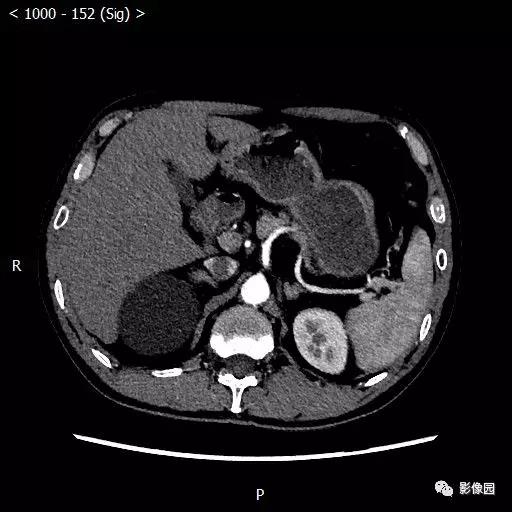
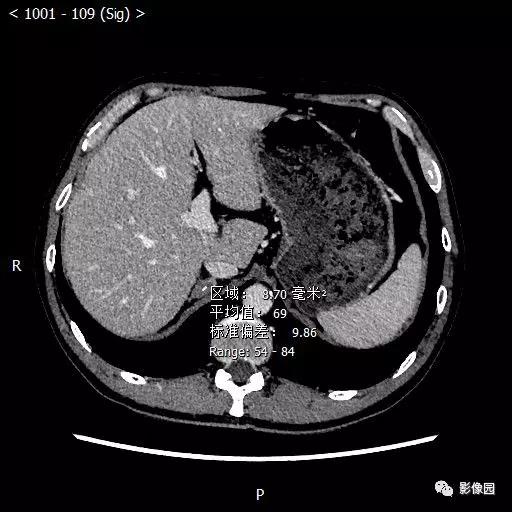
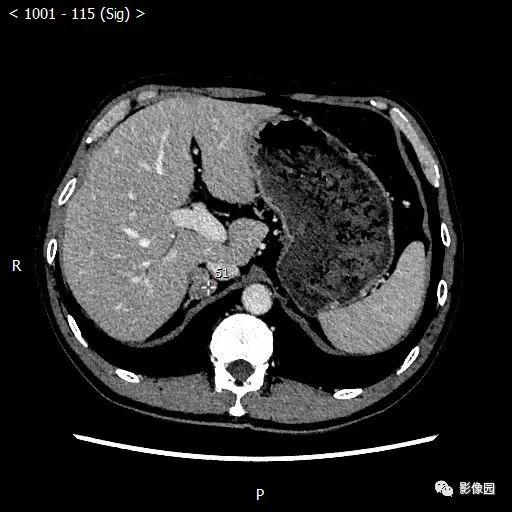
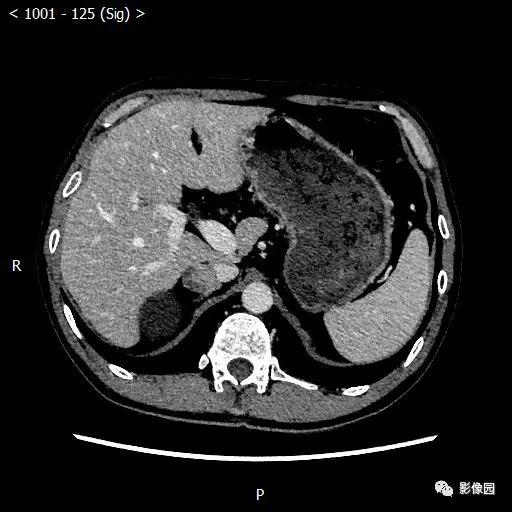
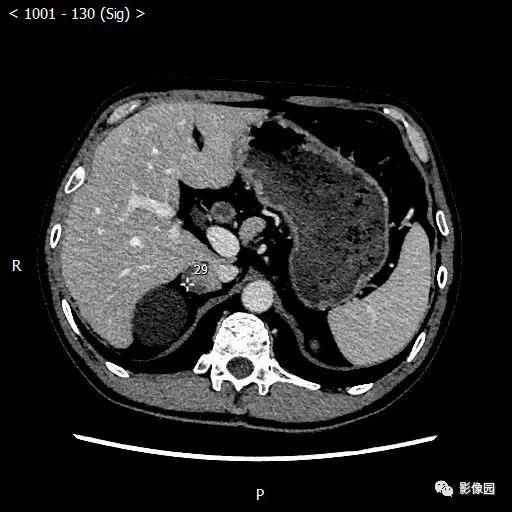
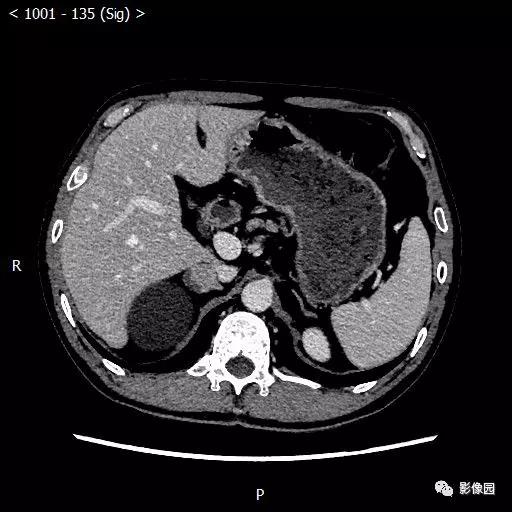
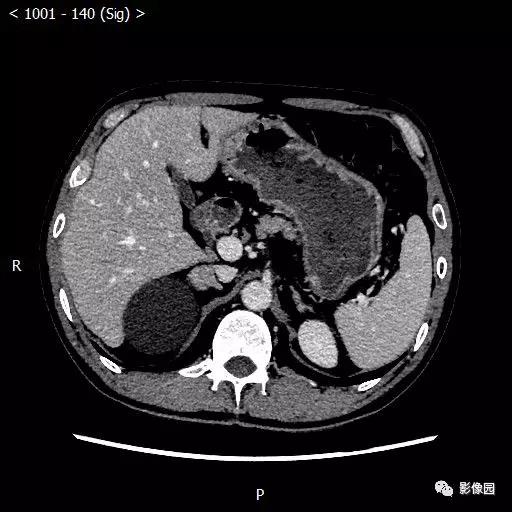
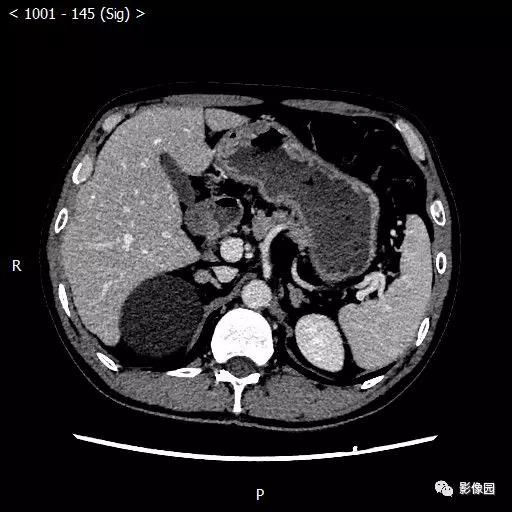
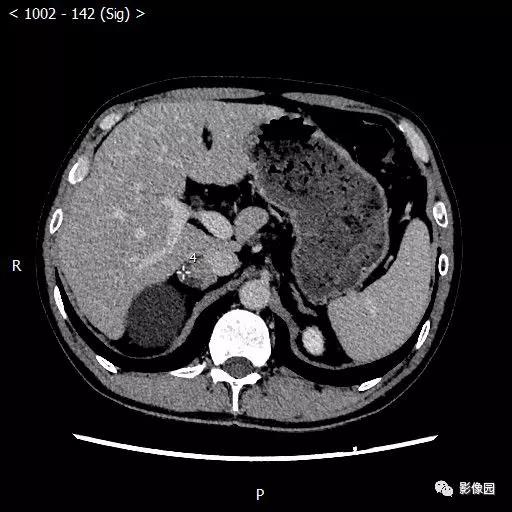
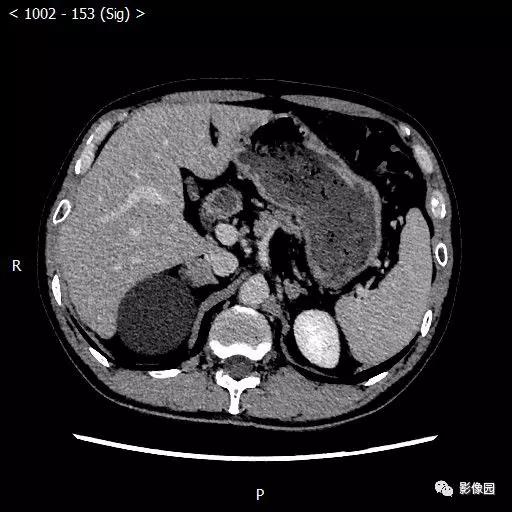
【影像图片】







【讨论】
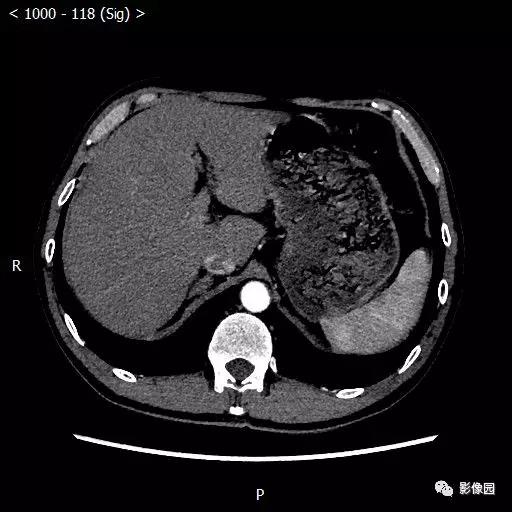
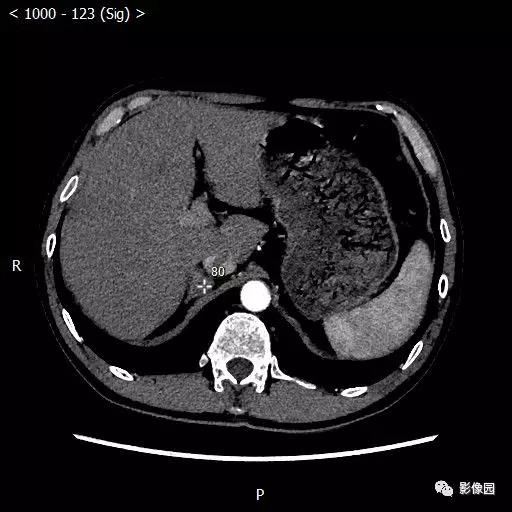
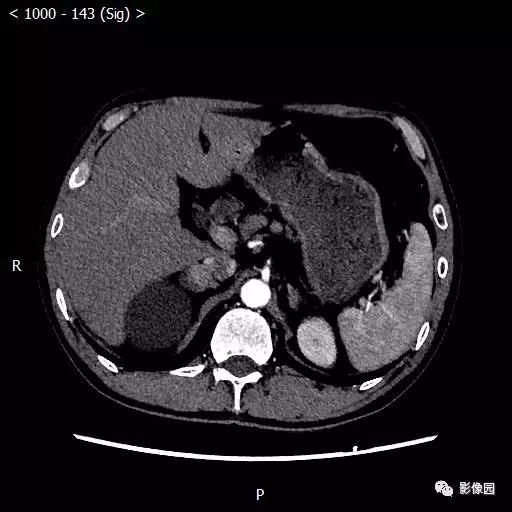
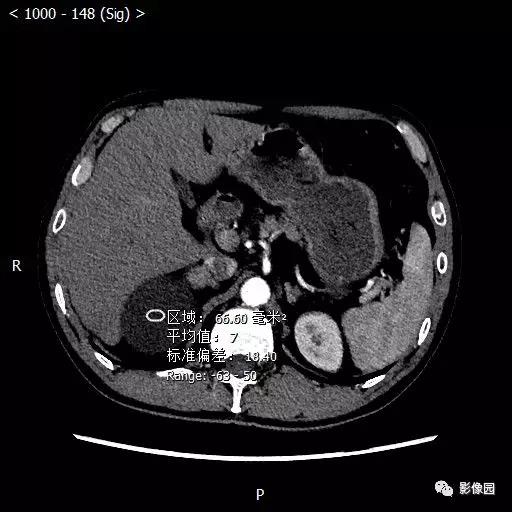
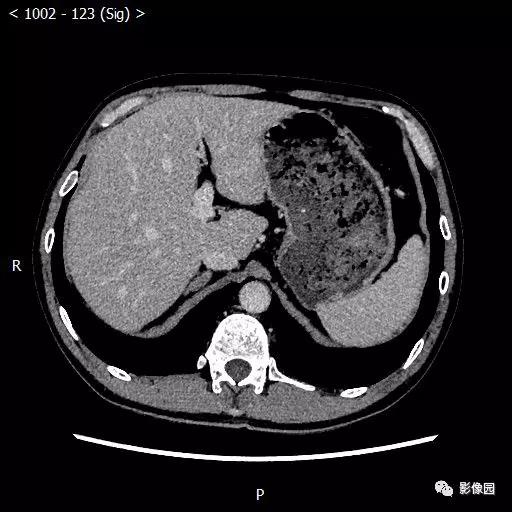
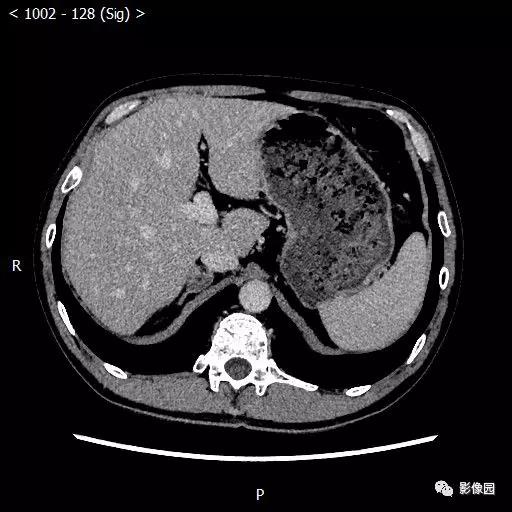
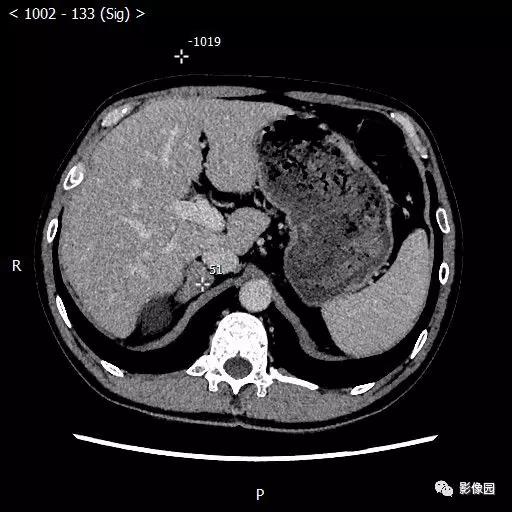
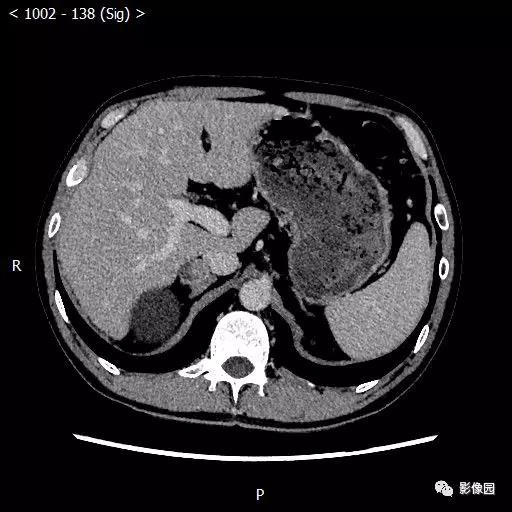
评论:右肾上级可见类圆形低密度影,CT值约7Hu,增强扫描未见强化。右肾上腺区见类圆形混杂密度影,增强扫描软组织成分呈中度强化。右肾上腺肿块,腺瘤?
【结果】
病理诊断:(右肾上腺肿物)符合肾上腺皮脂腺瘤。
【病例小结】
肾上腺腺瘤一般多单发,形态规整,边界清晰光滑,为圆形或类圆肿块,密度均匀,多为等密度病灶,但也可呈稍低密度。常有完整的包膜,增强后可轻度强化或不强化。根据分泌的激素不同,临床上可产生不同的症状,可分为:醛固酮增多症(Corm’s综合症)、皮质醇增多症(Cushing综合征)以及无功能性肾上腺腺瘤。醛固酮腺瘤起源于肾上腺皮质束状带,分泌过多糖皮质激素,以肥胖、多毛等为主要临床症状。皮质醇腺瘤起源于肾上腺皮质球状带,分泌过醛固酮激素,临床表现为高血压及高钠低钾等。腺瘤绝大部分属功能性肿瘤,非功能性肿瘤只占3%。皮质醇腺瘤体积略大,因为肾上腺皮质内束状带所占范围明显大于球状带,CT值略高,约30~50HU,增强扫描轻到中度增强。常合并有脂肪肝,且同侧或对侧肾上腺多有萎缩。而醛固酮瘤相对较小,一般1cm左右,由于其内富含脂质的透明细胞,所以密度低,CT值为0~30左右,甚至可为负值,增强后轻微强化或不强化。无功能腺瘤无特征性CT表现,定性诊断较困难,常需病理证实。对于有典型Corm综合症或Cushing综合征临床表现的皮脂腺瘤的诊断并不困难,但无症状的无功能腺瘤需与转移癌鉴别。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肾上腺#
36
#老年男性#
21
#肿物#
18