ASCO 2016:奥拉帕利(Olaparib)全面开战:卵巢癌、乳腺癌、胃癌
2016-06-10 肿瘤资讯 肿瘤资讯
Abstract 5501 Study19研究:Olaparib治疗BRCA突变铂敏感复发的浆液性卵巢癌的总生存期(OS)数据更新报道 Oral Abstract Session 背景: II期研究Study19显示,olaparib维持治疗对比安慰剂,可以显著延长铂敏感复发的高级别浆液性卵巢癌患者的无进展生存期(PFS),其中BRCA1/2基因突变(BRCAm)的患者接受ola
Abstract 5501 Study19研究:Olaparib治疗BRCA突变铂敏感复发的浆液性卵巢癌的总生存期(OS)数据更新报道 Oral Abstract Session
背景: II期研究Study19显示,olaparib维持治疗对比安慰剂,可以显著延长铂敏感复发的高级别浆液性卵巢癌患者的无进展生存期(PFS),其中BRCA1/2基因突变(BRCAm)的患者接受olaparib治疗获益更大。截至2012年11月26日的数据分析显示,olaparib对比安慰剂未能显著延长患者的总生存(OS):全分析集FAS(58% 数据成熟; HR 0.88, 95% CI 0.64–1.21,P =0.44),BRCAm亚组 (52%数据成熟; HR 0.73, 95% CI 0.45–1.17, P= 0.19) (Ledermann et al, Lancet Oncol 2014).本次,我们汇报进一步的生存数据(77%数据成熟,截止日期2015年9月30日)。
方法:患者1:1随机接受Olaparib(400 mg bid, 胶囊)或安慰剂治疗,其中,96%(254/265)的入组患者BRCA突变状态明确。
结果:无论是FAS还是BRCAm亚组,接受Olaparib相比于安慰剂组,均显示出了OS优势;FAS集患者的生存获益可能主要由于BRCAm患者的OS获益所致。
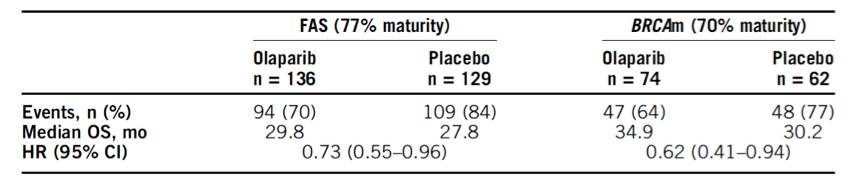
在FAS人群,Olaparib和安慰剂组5年的生存率分别为29.2%和20.4%;BRCAm亚组,5年的生存率分别为36.9%和24.3%. 截至2015年9月30日,Olaparib组15例(BRCAm 8例)和安慰剂组1例(BRCAm 1例)仍在接受治疗。Olaparib组中,13.2%(18/136)的患者接受了5年以上的Olaparib治疗(其中,BRCAm患者11例;non-BRCA突变患者7例)。安全性数据与既往报道一致。
结论:Study19研究的进一步随访数据显示,铂敏感复发的卵巢癌接受Olaparib维持治疗可以获得生存获益,Olaparib耐受性可,可用于长期维持。
Abstract 4041 Olaparib治疗晚期胃癌(AGC)的疗效预测生物标志物分析 Poster Session
背景:II期临床研究Study39入组了124例AGC患者,研究结果显示,无论是整体人群还是ATM低表达(ATMlow)的患者,二线Olaparib联合紫杉醇序贯(O/P组)对比紫杉醇(P)单药,可以显著延长患者的OS (Bang et al JCO 2015)。本研究探索性分析了其他潜在的生物标志物与ATM表达水平及临床疗效的关系。
方法:收集入组患者的肿瘤组织标本,进行二代基因测序并结合全基因组分析。潜在的生物标志物包括:微卫星不稳定样状态(MSI-like status,即总突变负荷 overall mutation load),ATM突变,以及参与同源重组修复的其他基因突变(HRRm)、TP53和ARID1A突变。研究入组时采用IHC检测患者的ATM表达水平。分析基因标志物间的相关性及各基因标志物与临床疗效的关系。
结果:124例研究者中,55例患者(ATMlow, n = 28; ATM positive [+ve], n = 27)有≥1个组织标本可以进行肿瘤基因组分析(evaluable for tumor genetics, EFTG)。其中,6例患者(11%)合并ATM功能缺失突变(均为ATMlow),35例(64%)患者合并TP53突变(TP53m)。HRRm(包括ATM)、ARID1A突变和MSI-like患者各为11、19和7例,这些患者多数为ATMlow。不同突变类型患者接受O/P vs P治疗的总生存(OS)风险比HR如下表:

虽然,本研究分析人数较少,但该探索性分析提示:1)ATMlow患者(无论TP53突变状态)接受O/P治疗,OS最长;2) ATMlow的患者,其死亡风险比均低于其他生物标志物;3) O/P组,无ATM突变的患者OS更长。
结论:对于AGC患者,ATM表达水平仍然是预测Olaparib疗效的最佳生物标志物。
Abstract 1080 Olaparib联合艾瑞布林用于蒽环和紫衫类化疗失败后的晚期三阴性乳腺癌(TNBC)的II期研究结果报告 Poster Session (Board #185)
背景:晚期TNBC患者相比于其他亚型的患者预后较差,缺乏有效的治疗靶点。艾瑞布林是晚期TNBC患者的标准治疗手段;Olaparib在胚系(g)BRCA1/2突变的患者中显示出较好的疗效。我们进行了该I/II期研究,期望艾瑞布林联合Olaparib用于晚期TNBC能产生协同治疗效应(无论患者BRCA1/2突变状态)。
在去年的ASCO大会上,公布了该研究的I期研究结果,Olaparib的推荐剂量为300mg,bid,本次汇报II期研究的结果,联合方案的疗效和安全性。
方法:本研究入组了蒽环和紫衫类化疗失败后的晚期TNBC患者,入组时无需确认患者的BRCA1/2突变状态。根据I期研究结果,艾瑞布林的用法为IV,1.4mg/m2,D1和D8;Olaparib为口服,300mg,bid.主要研究终点为ORR。
结果:2014年6月-12月,共入组24例患者,入组患者中位年龄为46岁(Range:27-73),既往接受化疗的中位治疗线数为3线(Range:2-6)。16例(66.7%)患者合并有内脏转移;8例患者无内脏转移。艾瑞布林和Olaparib相对的剂量强度分别为74.9%和75.4%。ORR为37.5%(95% CI: 18.8–59.4),包括CR患者1例。mPFS为4.2 m (95% CI: 2.7–7.6),mOS未达到,11例患者死亡。严重不良事件(3-4度)主要包括:白细胞减少(83.3%)、中性粒细胞减少(83.3%)、粒缺性发热(33.3%)、贫血(37.5%)和血栓形成(8.3%)。
结论:在晚期TNBC中,艾瑞布林联合Olaparib显示了较好的疗效,耐受性可。后续将探索性分析gBRCA1/2突变状态和同源重组修复缺失(HRD)和联合方案疗效的关系。
TPS1096 II期研究GeparOLA 方案报告:HER2阴性同源重组缺陷(homologous recombination deficiency,HRD)的早期乳腺癌新辅助治疗方案探索:Olaparib联合紫杉醇对比紫杉醇卡铂,序贯表阿霉素和(EC)Poster Session (Board #201a)
背景:目前,Olaparib用于同源重组缺失评分高(HRD score high)和/或(体细胞或胚系)BRCA1/2突变乳腺癌患者中的疗效仍然未知,此外,Olaparib联合化疗的毒副反应数据也很少。从GeparSixto和CALBG 40603研究中,我们看到,含卡铂的新辅助治疗方案,可以提高TNBC患者的pCR率,并且,gBRCA1/2突变和HRD score high的患者,pCR率(ypT0/isypN0)亦较高,分别为65%和63%。因此,我们设计了GeparOLA研究,旨在探索Olaparib用于HRD(BRCA1/2突变和/或HRD score high) HER2-早期乳腺癌的疗效。
治疗方法:GeparOLA研究将入组102例患者,随机1:1分配接受:紫杉醇80mg/m2每周方案(Pw)联合Olaparib 100mg bid (PwO),12周或Pw联合卡铂(Cb, AUC2,qw),(PwCb),12周。两组均序贯EC化疗。
分层因素包括:HR状态(HR+ vs HR-)、患者年龄(<40 vs ≥40)。
入组条件:1. 初治cT2-cT4a-d或cT1c(cN+或pNSLN+或HR-或ki67>20%); 2.g/t BRCAm或HRD high score。
主要研究终点:pCR率(ypT0/isypN0);次要研究终点:不同定义的pCR率(ypT0 ypN0; ypT0ypN0/+; ypT0/is ypN0/+; ypT(any) ypN0);保乳率;药物耐受性和安全性。
探索性分析:二代测序检测到的相关胚系和肿瘤突变与pCR的关系。
统计学分析:若pCR率≤55%,将不再进行III期临床研究(α= 0.1; 80%检验效能);假设pCR率为70%,PwO组患者数为65例,若pCR率≥65%(95%CI不包括55%),则能达到阳性结果。根据既往研究结果,PwCb组的pCR率约为50-60%。
结果:研究将于2016年在德国40-50个中心开始入组。
结论:GeparOLA研究旨在探索,在HRD的 HER2-早期乳腺癌新辅助治疗中,紫杉醇联合Olaparib对比紫杉醇联合铂类方案,何者pCR率更高。
Abstract 3015 抗PD-L1单抗Durvalumab (MEDI4736;D)与PARP抑制剂Olaparib(O)或VEGFR抑制剂Cediranib(C)联合治疗女性癌症:I期研究 Poster Discussion Session; Displayed in Poster Session (Board #337)
背景: O和C单药在复发卵巢癌中显示出了较好的疗效。研究假设,O和C联合D可以增强D的抗肿瘤活性(通过抑制DNA修复和诱导低氧等增加DNA损伤)。该I期临床研究评估了D+O和D+C两个联合的安全性和初步疗效。
方法:D+O组:O(200或300mg bid)+D 10 mg/kg IV , 14d/次 (剂量水平dose level [DL] 1, 2);O 300mg,bid+D 1500mg IV,28d/次(DL3)。D+C组:C(20或30mg qd)+D 10 mg/kg IV , 14d/次 (DL1, 2)。
结果:共入组19例患者,中位年龄66岁(39-70),既往中位治疗线数:4线(2-7)。
D+O组:10例卵巢癌(OvCa)、2例TNBC。3-4度AE包括:淋巴细胞减少(n=2)、贫血(n=1)。在9个可评估疗效的患者中,1例PR(PFS6+m)、5例SD(PFS4+m),疾病控制率DCR为67%,所有患者均为BRCA野生型。
D+C组:4例OvCa、2例宫颈癌、1例子宫肉瘤,3-4度AE包括:高血压(n=2)、腹泻(n=2)、肺栓塞(n=2)、肺动脉高压(n=1)、淋巴细胞减少(n=1)。DL1组中,2例患者因C导致的肺栓塞停止治疗;1例患者因频发乏力和腹痛需要C减量;DL2组中,4例患者因频发乏力和腹痛和/或呼吸困难进行了剂量减量。在7例可进行疗效评估的患者中,2例PR、2例SD,DCR为57%.
结论:D+O(O 300 mg, bid + D1500 mg, q28d)联合方案耐受性可,在BRCA野生型的OvCa和TNBC患者中,显示出较好的疗效。目前在卵巢癌、TNBC、肺癌和前列腺癌的II期临床研究已经开始入组。D+C的新DLs将探索最佳联合剂量。
Abstract 5562 Olaparib联合AZD1775用于耐药实体瘤的Ib期研究Poster Session (Board #385)
背景:细胞周期G1/S检查点缺失的肿瘤依赖Wee1 激酶在G2/M修复受损的DNA,从而阻止细胞周期延长。AZD1775Wee1 激酶的有效抑制剂。PARP抑制剂olaparib可以在S期导致DNA双链的断裂,假设联合Wee1 激酶抑制剂和PARP抑制剂可以有效杀灭癌细胞。本研究的主要目的在于探索AZD1775联合olaparib用于耐药实体瘤的最大耐受剂量(MTD)。
方法:入组成年耐药实体瘤患者,给药方式为: AZD1775(po,bid,d1-3和d8-10,21d/cycle),olaparib(po,bid,d1-14,21d/cycle)。
结果:共入组6例患者(男性1;女性5;中位年龄59岁),分配进入两个研究队列:AZD1775 125 mg (n=3)或AZD1775 150 mg (n=3),所有患者接受olaparib的剂量为100mg。患者接受的中位治疗周期为3个周期(Rang:2-6)。未观察到MTD。不良事件(AE)包括:恶心、腹泻(n=4),咳嗽、乏力、便秘、肌肉痉挛、潮热、血小板减少(n=2),贫血、头痛、手足疼痛、背痛(n=1)。疗效评估:1例PR(肛门癌)、4例SD、1例PD.
目前研究正在进行队列3入组:分为2组,Arm1: AZD1775 175 mg olaparib 100 mg; Arm 2: AZD1775 150 mg+ olaparib 200 mg.
结论:该I期研究探索了AZD1775联合olaparib方案,并观察到早期的安全性和疗效数据。待最佳的剂量和给药方式确定后,将在更多瘤种中进行拓展试验。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#olaparib#
32
#乳腺癌、#
47
#ASC#
41
#LAP#
47
奥拉帕尼联用紫杉醇治疗晚期胃癌/胃食管结合部癌患者的Ⅲ?期试验?GOLD?研究,由于未达到主要终点:改善患者总生存,而宣告失败。
142
#APA#
0
这个不错
122
值得研究
130
只要有brca1突变都可以使用
97