脾硬化性血管瘤结节性转化CT和MRI表现一例
2019-11-22 杜倩 鲍柱擎 临床放射学杂志
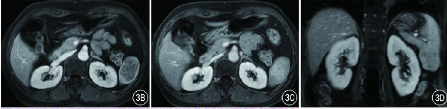
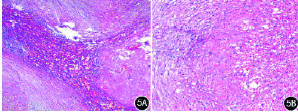
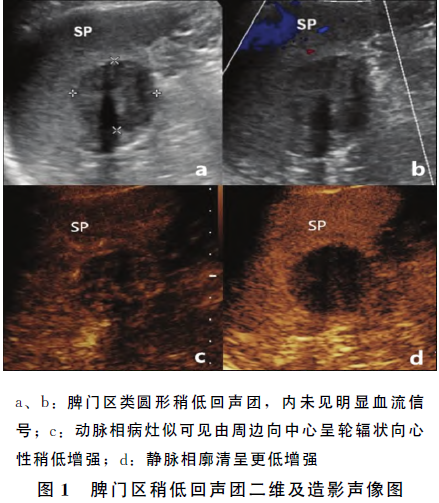
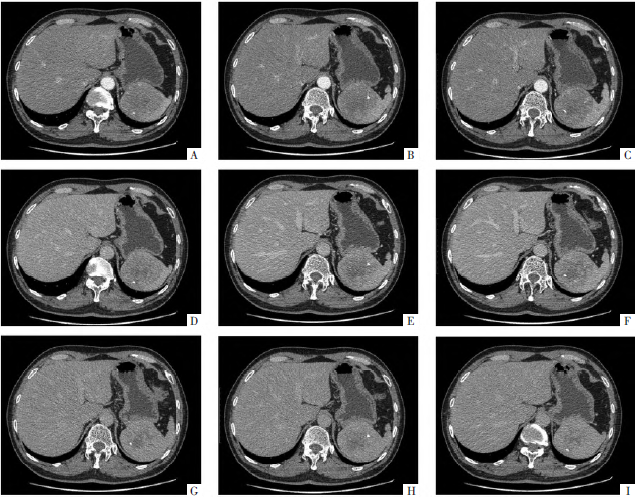
患者女,54岁。因“右侧结节性甲状腺肿”来院就诊,入院行CT增强检查示脾下极见一约2.9 cm×3.4 cm×4.4 cm团块状稍低密度影,密度均匀,边界清楚,周围似可见包膜,增强扫描病灶呈渐进性强化,延迟期病灶密度与脾相近呈等密度(图1A~E)。MRI增强示脾下方肿块呈稍长T1、稍短T2信号,信号欠均匀,边界清楚。扩散加权成像(DWI)呈低信号。增强扫描肿块动脉期强化不明显,门静脉至延迟期呈渐进


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#脾硬化性#
33
#结节性#
36
#血管瘤#
0
#硬化性#
26