Sci Transl Med:克服HER2靶向癌症治疗耐药的新策略-中国研究者祁小龙博士点评
2017-05-26 肿瘤资讯 肿瘤资讯
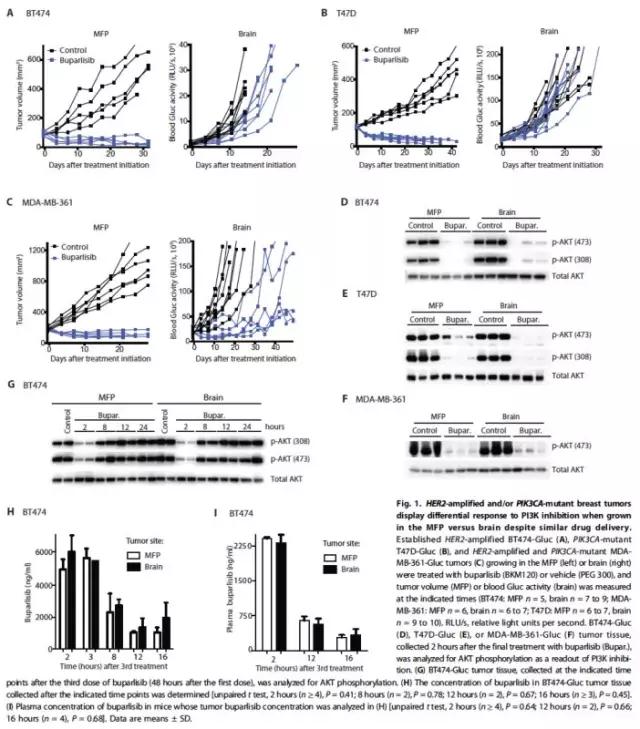
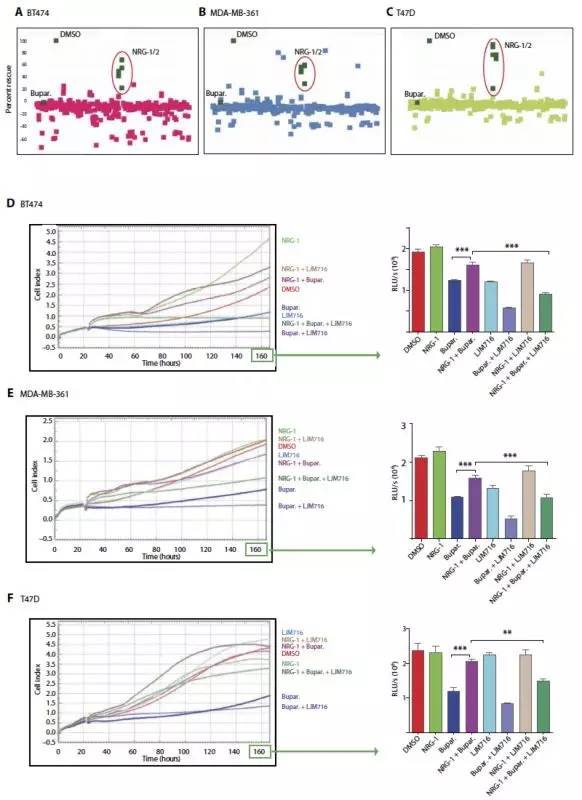
5月24日,Science旗下权威期刊Science Translational Medicine(影响因子16.264)以封面文章Cover story刊登了哈佛大学麻省总医院Rakesh K. Jain(美国科学院院士、美国工程院院士)团队的研究成果“The brain microenvironment mediates resistance in luminal breast cancer

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究者#
39
#TRA#
24
#癌症治疗#
25
#Transl#
27
#新策略#
24
#Med#
29
学习了。。。。。。。。
71