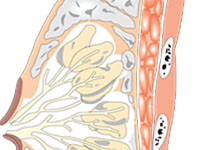
Lancet oncol:肿瘤浸润淋巴细胞(TIL)与不同亚型的乳腺癌预后的关系。
2017-12-08 MedSci MedSci原创
肿瘤浸润淋巴细胞(TILs)可预测三阴乳腺癌(TNBC)和HER2炎性乳腺癌对新辅助化疗的反应性,但其在导管性乳腺癌中的作用以及TILs对所有亚型预后的影响尚不是很清楚。近期Lancet子刊上发表一篇文章,研究人员对TILs与TNBC、HER2阳性乳腺癌和HER2阴性的导管性乳腺癌患者对化疗的敏感性和预后之间的关联进行评估。从德国乳腺癌学会所做的6个随机试验中筛选进行新辅助化疗的原发乳腺癌患者。初
对于HER2阴性的导管性乳腺癌亚型,低TILs、中TILs和高TILs患者获得病理性完全反应(pCR)的比例分别是6%(45/759)、11%(48/435)和28%(49/172)。对于HER2阳性乳腺癌亚型,低TILs、中TILs和高TILs患者获得pCR的比例分别是32%(194/605)、39%(198/512)和48%(127/262)。最后,对于TNBC乳腺癌亚型,低TILs、中TILs和高TILs患者获得pCR的比例分别是31%(80/260)、31%(117/373)和50%(136/273)(所有亚型p<0.0001)。在单变量分析中,TILs增加10%,即可延长TNBC和HER2阳性乳腺癌患者的无进展存活期(TNBC:危险比[HR]0.93[95% CI 0.87-0.98],p=0.011;HER2+:0.94[0.89-0.99],p=0.017),但对HER2阴性的导管性乳腺癌则无明显影响(1.02[0.96-1.09],p=0.46)。TILs增加,还可延长TNBC患者的总体存活期(0.92[0.86-0.99],p=0.032),但对HER2阳性的乳腺癌患者的存活期无明显影响(0.94[0.86-1.02],p=0.11),此外,TILs增加,与HER2阴性的导管性乳腺癌患者总体存活期缩短相关(1.10[1.02-1.10],p=0.011)。
Carsten Denkert,et al.Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy.The Lancet Oncology.07 December 2017. http://dx.doi.org/10.1016/S1470-2045(17)30904-X
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Lancet#
26
#Oncol#
0
一起学习一下
81
#淋巴细胞#
31
非常好的文章.学习了
66