NEJM:Nivolumab一线应用对生存的改善不优于标准化疗(CheckMate 026研究)
2017-06-23 李刚 全球肿瘤快讯杂志
美国俄亥俄州立大学综合癌症中心David P. Carbone等报告,针对初治的Ⅳ期非小细胞肺癌(NSCLC)患者、或PD-L1表达≥5%的复发性患者,Nivolumab对比含铂化疗并未显著改善患者的无进展生存期(PFS),且两种方案治疗后患者的总生存(OS)获益相近;但Nivolumab的安全性优于化疗,且未见新发的或超出预期的安全事件。(N Engl J Med. 2017;376:241
美国俄亥俄州立大学综合癌症中心David P. Carbone等报告,针对初治的Ⅳ期非小细胞肺癌(NSCLC)患者、或PD-L1表达≥5%的复发性患者,Nivolumab对比含铂化疗并未显着改善患者的无进展生存期(PFS),且两种方案治疗后患者的总生存(OS)获益相近;但Nivolumab的安全性优于化疗,且未见新发的或超出预期的安全事件。(N Engl J Med. 2017;376:2415-2426.)
研究背景
过去20年中,虽然含铂化疗一直是无靶向药物敏感基因突变的、晚期NSCLC患者的一线标准方案。但既往多项Ⅲ期临床试验结果显示,铂类为基础化疗治疗NSCLC时仅能获得4~6个月的中位PFS及10~13个月的中位OS。随着免疫检查点抑制剂的出现,已有两项Ⅲ期研究证实:在含铂化疗后疾病进展的转移性NSCLC患者中,Nivolumab复治NSCLC患者较多西他赛可获得更长的总生存期。这种生存获益虽然与PD-L1的表达状态无关,但PD-L1表达增高的非鳞癌型NSCLC患者经Nivolumab治疗后生存获益更大。
鉴于免疫系统的复杂性,既往研究者们探索了PD-L1表达水平之外的疗效预测标志物的情况。早期数据支持“肿瘤负荷高可增加免疫治疗获益可能性”的假设。
研究详情
为了明确Nivolumab对比化疗的疗效和安全性,该项代号为CheckMate 026的国际、随机化、开放标签的Ⅲ期临床试验入组了1325例含铂化疗Ⅳ期或一线治疗后的复发性NSCLC患者,只有入组前6个月内的新鲜或存档肿瘤组织样本的PD-L1表达水平≥1%才予以随机化分组。541例(41%)患者按照1:1的比例接受随机化分组(271例被分入Nivolumab组,治疗方案为Nivolumab 3 mg/kg,q14;270例被分入研究者选择的含铂双药化疗组,治疗方案为q21,最多治疗6个周期),另784例(59%)患者因PD-L1表达情况无法评估(6%)、PD-L1表达<1%(23%)或不符合其他的入组条件(30%)而未被随机化分组。化疗组患者可在疾病进展后交叉至Nivolumab组。主要研究终点为PFS,由独立中心在PD-L1表达≥5%的患者中盲法评估得出。
此外,研究者还探索性分析了肿瘤突变负荷对临床结局的影响。肿瘤突变负荷的定义为:基线肿瘤样本中存在体细胞错义突变的总量,且经全外显子测序法在肿瘤组织样本和血样中予以证实。其中0~100个突变为低负荷组,100~242个突变为中度负荷组,≥243个突变为高负荷组。
主要疗效分析结果
主要疗效分析在423例PD-L1表达≥5%的患者群体中开展。虽然两组患者的基线临床特征在随机化时已被均衡,但Nivolumab组女性患者比例(32% vs 45%)、PD-L1表达≥50%患者的比例(32% vs 47%)均低于化疗组的,肝转移比例(20% vs 13%)高于化疗组的。此外,Nivolumab组靶病灶合并计算的肿瘤负荷更大。
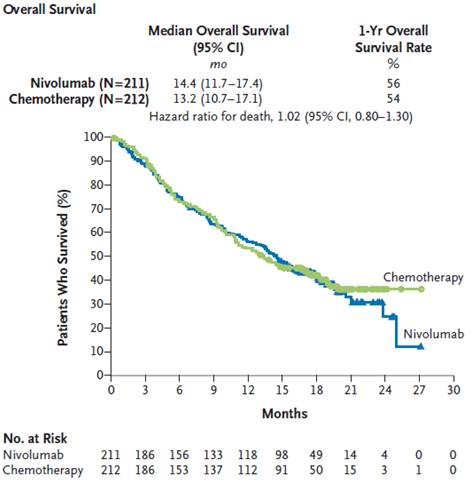
结果显示,423例PD-L1表达≥5%的患者的中位PFS在Nivolumab治疗组为4.2个月,在化疗组的为5.9个月(HR=1.15,95%CI0.91~1.45;P=0.25),中位OS分别为14.4个月和13.2个月(HR=1.02,95%CI 0.80~1.30)(见图1和图2)。化疗组的212例患者中共有128例(60%)交叉至Nivolumab组接受后续治疗。
图1 Nivolumab组和化疗组患者的PFS
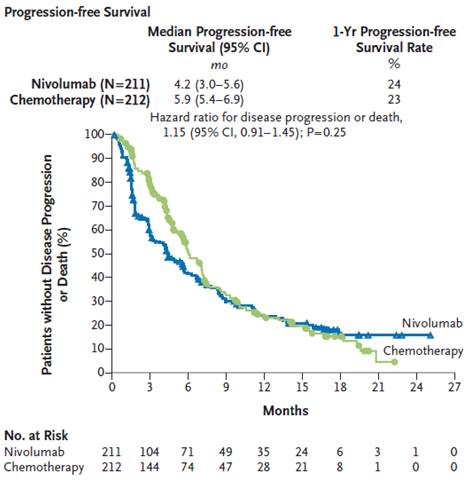
图2 Nivolumab组和化疗组患者的OS
Nivolumab组患者任何级别治疗相关不良反应事件的发生率为71%,而化疗组的为92%;3~4级治疗相关不良反应事件的发生率为18%和51%。
探索性分析结果
在PD-L1表达≥50%患者中开展的探索性亚组分析显示,Nivolumab组和化疗组患者的缓解率分别为34%(95%CI24%~45%)和39%(95%CI30%~48%),值得注意的是:该研究方案中并未针对PD-L1表达是否≥50%而对患者进行分层,且该情况下两组女性患者的比例并不均衡。
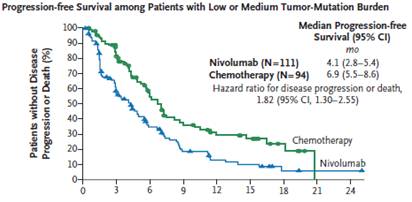
在312例(随机分组患者占58%)患者中,探索性分析评估了肿瘤突变负荷对临床结局的影响(图3和图4)。虽然两个随机分组患者基线时的肿瘤负荷并不均衡,但这些数据及生存结果在入组总人群中是一致的。在肿瘤突变负荷较高的患者中,Nivolumab组和化疗组患者的缓解率分别为47%和28%,中位PFS分别为9.7个月和5.8个月(HR=0.62,95%CI 0.38~1.00)。中位OS相似,不受肿瘤突变负荷的影响。不过,化疗组有68%的肿瘤突变负荷高的患者交叉至Nivolumab组接受治疗。
图3 Nivolumab组和化疗组高肿瘤突变负荷患者的PFS

图4 Nivolumab组和化疗组低~中度肿瘤突变负荷患者的PFS
虽然仅肿瘤突变负荷高、仅PD-L1表达≥50%、两种因素均有、两种因素均无的患者接受Nivolumab治疗后可分别获得32%、34、75%和16%的缓解率,但数据比较的统计效能不足。
原始出处:
Carbone DP1, Reck M1, Paz-Ares L et.al. First-Line Nivolumab in Stage IV or Recurrent Non-Small-Cell Lung Cancer.N Engl J Med. 2017 Jun 22;376(25):2415-2426. doi: 10.1056/NEJMoa1613493.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#标准化疗#
28
#mAb#
0
#Checkmate#
28
#NIV#
22
#标准化#
30
学习了,谢谢分享
59