Asian Pac J Allergy Immunol:患有或不患有过敏性鼻炎的哮喘儿童中,Th17细胞调控的免疫应答比较
2018-04-07 AlexYang MedSci原创
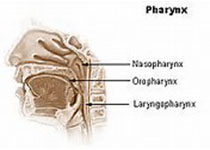
最近,有研究人员在患有或者不患有过敏性鼻炎的哮喘儿童中,调查了Th17细胞调控的免疫应答是否具有差异。研究人员在儿童中进行了一个案例-对照比较试验,其中包括67名哮喘(AS)儿童,50儿童患有过敏性鼻炎,52名儿童同时患有AS和AR(ASR),25名为传染性鼻炎(IR)和55名健康对照(HC)。研究人员使用的技术包括流式细胞仪、酶联免疫吸附试验等。研究发现,组内比较阐释了Th17细胞在ASR组中水
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Th17细胞调控#
35
#Asian#
36
#过敏性#
38
#ASIA#
32
#ALL#
38
#免疫应答#
38
#Th17#
43
谢谢分享学习了
58