Blood:免疫调节剂(IMiDs)通过促进Ikaros/Aiolos降解来上调CD38,进而增强达雷木单抗介导的骨髓瘤细胞杀伤
2018-09-20 MedSci MedSci原创
中心点:Ikaros和Aiolos失活可再现IMiDs在MM中的细胞内在作用以及转录变化。Ikaros或Aiolos缺失可上调干扰素刺激基因,包括CD38。摘要:近期有研究表明免疫调节药物(IMiDs)可促进转录因子Ikaros和Aiolos降解。但是,Ikaros和Aiolos缺失为何可导致多发性骨髓瘤(MM)细胞死亡尚不明确。Pasquale L. Fedele等研究人员采用CRISPR-Ca
Ikaros和Aiolos失活可再现IMiDs在MM中的细胞内在作用以及转录变化。
Ikaros或Aiolos缺失可上调干扰素刺激基因,包括CD38。
摘要:
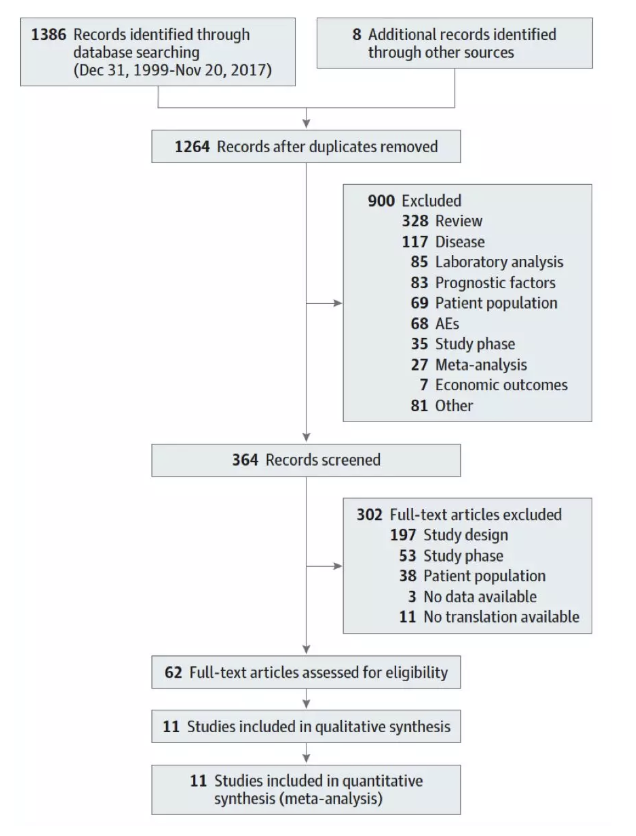
Pasquale L. Fedele等研究人员采用CRISPR-Case9基因编辑,建立敲除IKZF1/Ikaros和IKZF3/Aiolos敲除的人类MM细胞系,进一步研究其下游基因的调控网络。结果显示任一种失活均可再现IMiDs的细胞内在作用,导致细胞周期阻滞和诱导细胞凋亡。
此外,转录谱分析显示Ikaros或Aiolos失活与来那度胺治疗的效果有显著的重叠。这些效果并不依赖IRF4-MYC轴的降低,因为在细胞死亡过程中两种蛋白均无持续降低,加上过表达任一种细胞因子都不能恢复Ikaros丢失。
重要的是,Ikaros和Aiolos抑制干扰素刺激基因(ISGs,包括CD38)的表达,其缺失可激活干扰素样反应,导致MM细胞死亡。Ikaros/Aiolos通过与核小体重构和脱乙酰酶复合物相互作用,抑制MM细胞的CD38表达。IMiD诱导Ikaros缺失或干扰素治疗均导致MM细胞表面的CD38表达增加,从而启动达雷木单抗诱导的NK细胞介导的抗体依赖性的细胞毒性作用。
综上所述,本研究进一步揭示了IMiDs的作用机制,为联合抗CD38单克隆抗体治疗提供机制理论。
Pasquale L. Fedele,et al. IMiDs through loss of Ikaros and Aiolos primes myeloma cells for daratumumab mediated killing by upregulation of CD38. Blood 2018 :blood-2018-05-850727; doi: https://doi.org/10.1182/blood-2018-05-850727
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Aiolos#
41
#IMiDs#
35
#Ikaros#
47
学习了,谢谢作者分享/
79
#ROS#
38
#达雷木单抗#
0
学习了,谢谢分享
55
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
87