【一般资料】
患者男,49岁
【主诉】
因"咳嗽、气促,咳白色黏液痰,每日30~40ml"于2014年12月3日入院
【现病史】
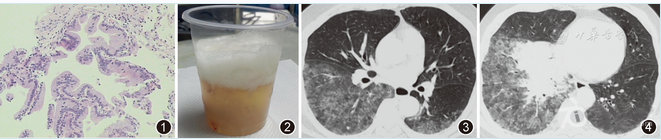
经PET-CT及支气管镜肺组织活检诊断为双肺黏液腺癌,TNM分期属于T4N2M0期(图1)。于2014年12月11日开始进行5个疗程的化疗(TP方案:紫杉醇+顺铂),前4个疗程后患者症状好转,咳痰减少,气促减轻,病灶缩小。第5个疗程后患者痰量较前增多,80~120ml/d,气促加重,复查胸部CT提示病灶进展。于2015年3月31日开始改为盐酸埃克替尼125mg,口服,3次/d。服药后6个月内患者咳痰减少,气促减轻,病灶缩小。从第7个月开始出现咳嗽、咳痰加重,咳大量水样黏液泡沫痰(图2),量多时可达2L/d,伴发热1周,于2015年10月10日再次入院。
【体格检查】
脉搏114次/min,呼吸32次/min,血压103/64mmHg(1mmHg=0.133kPa),SPO2为86%(吸氧浓度5L/min)。皮肤及口唇发绀,双肺呼吸音粗,双下肺可闻及湿性啰音。
【辅助检查】
影像学提示病灶进展(图3,图4)。血气分析:pH值为7.448,二氧化碳分压为35.3mmHg,氧分压为43.7mmHg。血清钾为4.4mmol/L,血清钠为102.4mmol/L,血清氯为66.3mmol/L。
【治疗】
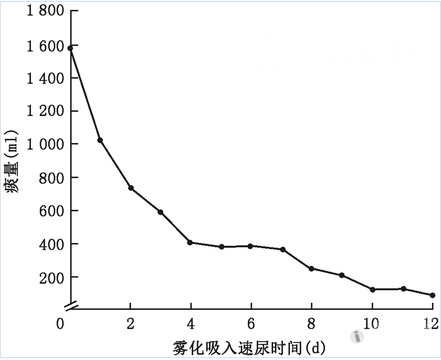
入院后给予无创通气[S/T模式,吸气相正压(IPAP)为19cmH2O(1cmH2O=0.098kPa),呼气末正压(EPAP)为7cmH2O,吸氧浓度为80%],纠正电解质,抗感染等治疗,患者症状无明显改善,氧合指数250mmHg,咳少量白痰,住院第18天步行出院。
【讨论】
原发性肺黏液腺癌是肺腺癌的一种特殊亚型,临床少见,文献报道仅占肺腺癌的0.14%,其分化程度高,恶性程度低。病理特征为较多的黏液分泌并堆积在细胞中,将细胞核挤压到细胞的一侧呈新月形。细胞内可见大量黏液。癌细胞产生的大量黏液在细胞外形成大小不等的黏液湖。黏液腺癌比较典型的临床特征为咳大量水样黏液泡沫痰。临床上将24h产生的水样黏液痰超过100ml称为支气管黏液溢。有文献报道,支气管黏液溢最多时可咳出9L/d的水样黏液痰。支气管黏液溢可引起严重的低氧血症,临床上治疗经验较少。目前国内外报道的有关治疗原发性肺黏液腺癌(以及肺泡癌)支气管黏液溢方法的文献仅有10多篇,且大都为个案报道,疗效不一。文献中提到的方法有:(1)使用大环内酯类药物(阿奇霉素、克拉霉素及红霉素);(2)吸入激素(氟替卡松或倍氯米松);(3)吸入消炎痛;(4)使用奥曲肽;(5)抗胆碱能药物(阿托品或东莨菪碱);(6)表皮生长因子受体(EGFR)酪氨酸激酶抑制剂;(7)手术治疗。关于吸入速尿治疗支气管黏液溢的报道只有1995年日本1篇文献中提到口服红霉素和吸入倍氯米松治疗1例支气管哮喘并支气管黏液溢的患者,疗程为2个月余,咳痰症状反复,在上述治疗的基础上加用雾化吸入速尿15~30mg,1个月后患者痰量减少,痰液性状改善。原发性肺黏液腺癌如果化疗或靶向治疗无效,其产生的支气管黏液溢治疗非常棘手。支气管黏液溢不但可引起严重的低氧血症,大量的黏液分泌也会导致顽固的水电解质紊乱和机体脱水。本例患者除了难以纠正的低氧血症,也出现了严重的低钠、低氯血症。治疗原发性肺黏液腺癌引起的支气管黏液溢应首先治疗肿瘤,但如果对化疗等抗肿瘤治疗不敏感或不能耐受再次化疗的患者只能对症处理,抑制黏液分泌。黏液腺癌导致大量黏液分泌的机制有:(1)炎症刺激等多种因素导致产黏液细胞过度分泌;(2)支气管上皮细胞对氯离子通道转运增强,导致氯和钠分泌增多,伴随水的过度分泌;(3)各种炎性介质导致血管通透性增加,血浆渗透至气道增多,其中起主要作用的是氯离子通道转运增强。速尿是临床上常用药物,一般为口服或静脉注射给药。通过雾化吸入速尿治疗原发性肺黏液腺癌支气管黏液溢的可能机制有:(1)抑制支气管黏膜上皮细胞的氯离子通道,减少氯化物向气道内分泌,改善上皮细胞的水转移,减轻黏膜水肿;(2)速尿可调节前列腺素代谢,减少前列腺素对氯离子转运通道的促进作用;(3)速尿可抑制迷走神经,减少胆碱能等神经递质的释放;(4)稳定肥大细胞和其他炎症细胞,抑制炎症介质释放,减少腺体分泌,降低血管通透性;(5)影响气道上皮神经末梢感受器的活性,降低末梢神经细胞的兴奋性,其中阻断氯离子通道和抑制胆碱能神经递质的释放起到了主要作用。本例患者雾化吸入速尿后,痰量明显减少,氧合状态改善,未出现明显不良反应,为肿瘤的进一步治疗赢得了机会。雾化吸入速尿治疗支气管黏液溢方法简单、方便,但其机制应进一步探讨。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
25
#速尿#
39
#支气管#
26
学习
58
#雾化#
24
好病例.学习了.
44