张锋再造三合一组合抗病毒的新型CRISPR Cas13系统
2019-10-15 徐悦 生物探索
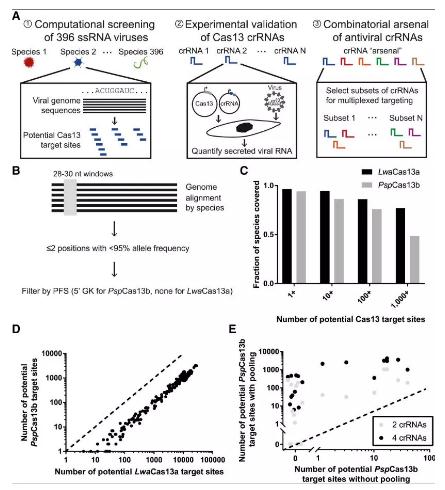
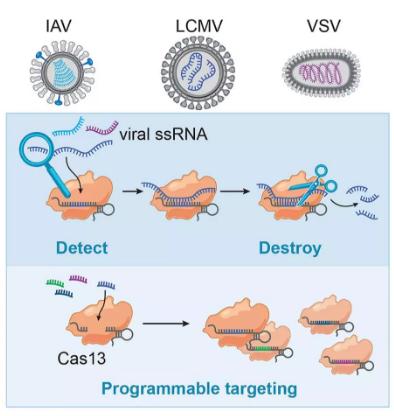
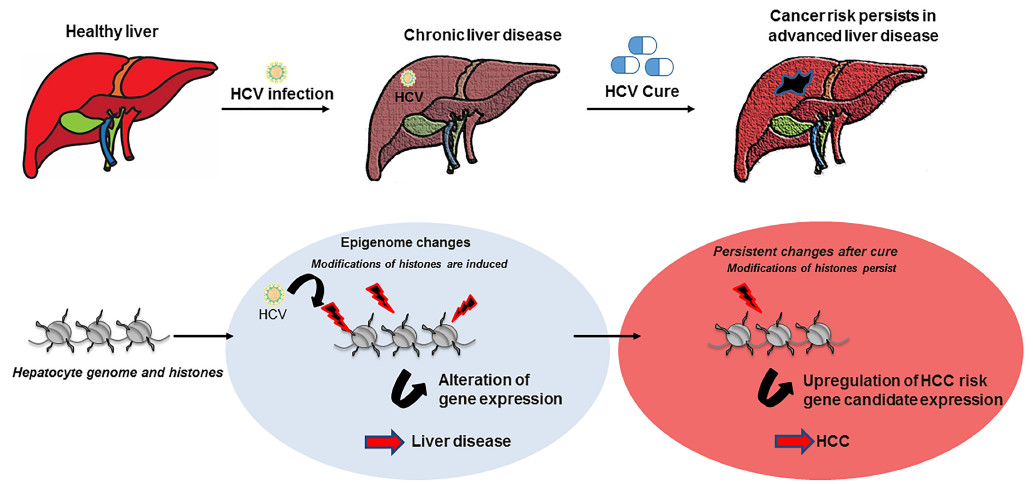
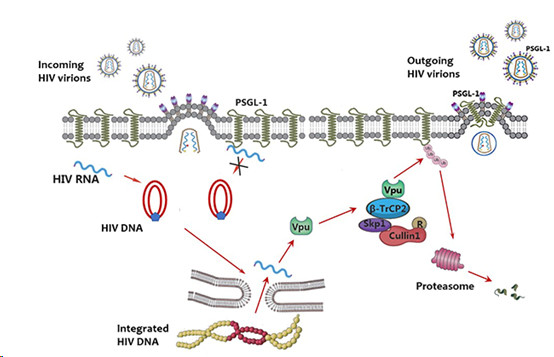
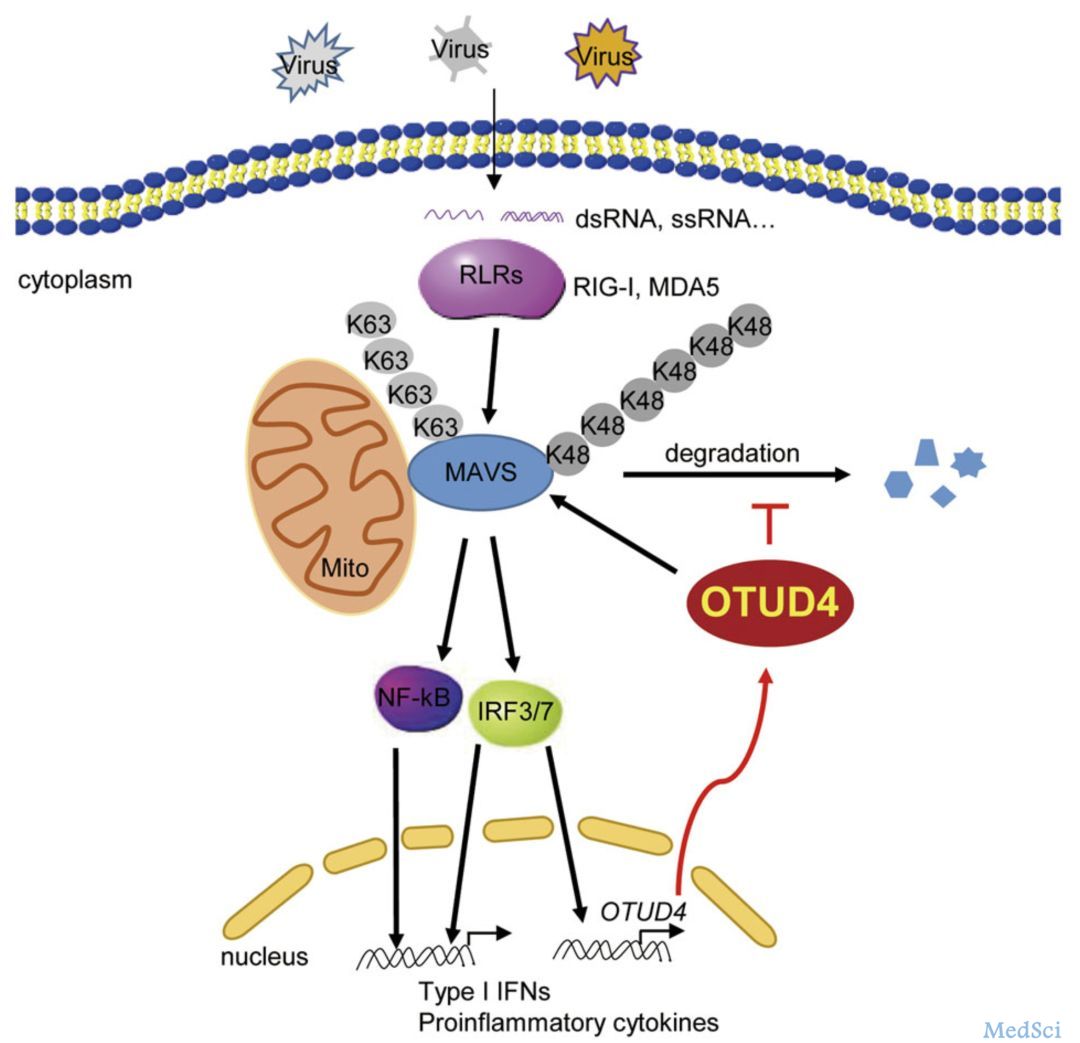
近日,麻省理工学院和哈佛大学Broad研究所传来好消息:Pardis C. Sabeti、张锋等科学家联合开发出一种新型的抗病毒系统。世界上有许多常见的致命病原体都是基于单链RNA的病毒,像是埃博拉病毒、寨卡病毒和流感病毒。该系统在CRISPR Cas13技术的基础上再次升级,可用于检测和破坏人类细胞中具有单链RNA的病毒。该研究发表在《Molecular Cell》杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cas13#
46
#Cas13系统#
27
#CRISPR#
31
#抗病毒#
26
#Cas#
26