刘文忠教授:全国第五次HP共识常见问题解读
2018-04-02 消化客 江苏省人民医院消化科
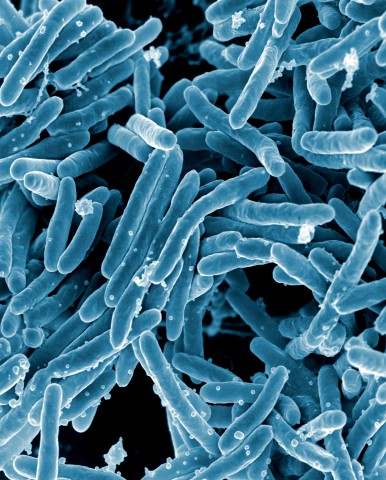
在江苏省医学会HP与胃肠道微生态学组成立大会上,来自上海仁济医院的刘文忠教授为我们解读了全国第五次HP共识常见问题。此次共识与国际接轨,突出了重点且更科学,但也可能出现内容的遗漏、操作性不佳等问题。刘教授针对HP根治与否、HP的检测、治疗及传播等问题做了相关的解读。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#常见问题#
35
学习了
69
学习了
79
学习.
71
学习了.幽门螺旋杆菌
0
学习了
71
不错的文章值得推荐
25