史上首次:日本确认iPS视细胞能让眼睛恢复感光
2017-01-13 佚名 中新网
据日媒报道,日本理化学研究所多细胞系统形成研究中心(位于神户市)的研究小组在本月10日的美国科学杂志网络版上发表一项研究成果,确认iPS视细胞能让眼睛恢复感光。 据报道,结果显示,研究者让诱导多能干细胞(iPS细胞)变为视网膜的视细胞,并移植到因晚期“视网膜色素变性症”失明的老鼠眼中,结果老鼠变得眼睛能够感光了。这是首次确认使用ips细胞能够恢复感光功能。 副项目带头人万代道子解释说
据日媒报道,日本理化学研究所多细胞系统形成研究中心(位于神户市)的研究小组在本月10日的美国科学杂志网络版上发表一项研究成果,确认iPS视细胞能让眼睛恢复感光。 据报道,结果显示,研究者让诱导多能干细胞(iPS细胞)变为视网膜的视细胞,并移植到因晚期“视网膜色素变性症”失明的老鼠眼中,结果老鼠变得眼睛能够感光了。这是首次确认使用ips细胞能够恢复感光功能。

副项目带头人万代道子解释说:“我认为现阶段是能感受到少许光亮,视野稍有拓宽的程度。”她计划也用人类ips细胞进行验证,在2年以内申请临床研究。
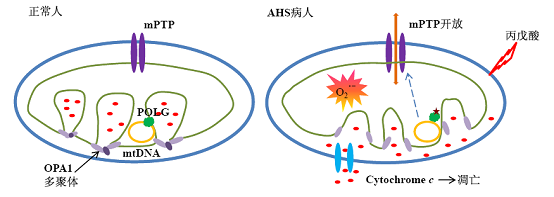
据悉,视细胞的功能是接收光亮,然后传递给视网膜的神经细胞。如果视细胞发生变性而消失,就会出现“视网膜色素变性”,造成视力减弱,甚至失明。
研究小组在实验中的做法是:在老鼠所在的房间有光亮5秒后就给予电击,让老鼠学会在感觉到光亮时,为了免遭电击而逃入相邻的房间。结果,因晚期“视网膜色素变性症”失明9只老鼠没有逃跑。
另一方面,研究小组把用ips细胞制作的视网膜前期组织移植到老鼠双眼中,令其变成视细胞。这样的10只老鼠中,有4只变得在房间有光亮后会逃走,恢复了感光功能。
报道还称,在该实验中,移植的部分不足全视野的5%。如果扩大移植范围,恢复率有可能增大。
研究小组的项目带头人高桥政代等2014年在全球首次使用ips细胞制作的视网膜色素上皮细胞,移植给因“渗出型老年黄斑变性”而视力减弱的患者,手术获得了成功。该手术虽然具有维持视力的效果,但从检查上未能确认是否恢复了感光功能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#视细胞#
27
继续学习中
65
#日本#
28
#iPS#
33
日本人牛啊
67