Lancet oncol:纳武单抗联合或不联合伊匹单抗治疗转移性肉瘤的效果和安全性。
2018-01-21 MedSci MedSci原创
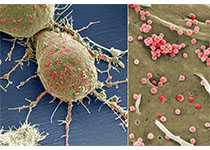
转移性肉瘤患者可选择的治疗方式有限。Nivolumab(纳武单抗)和ipilimumab(伊匹单抗)分别是靶向PD-1和CTLA-4的单克隆抗体。研究人员现对用纳武单抗单独或联合伊匹单抗用于治疗局部晚期、不可手术切除的或转移性肉瘤患者的效果和安全性进行研究。研究人员进行一多中心的、开放性的、非对比性的、随机2期研究,招募年满18岁的病理性确诊的肉瘤患者,且要求已有转移、或局部晚期、或不可手术切除,
转移性肉瘤患者可选择的治疗方式有限。Nivolumab(纳武单抗)和ipilimumab(伊匹单抗)分别是靶向PD-1和CTLA-4的单克隆抗体。研究人员现对用纳武单抗单独或联合伊匹单抗用于治疗局部晚期、不可手术切除的或转移性肉瘤患者的效果和安全性进行研究。
研究人员进行一多中心的、开放性的、非对比性的、随机2期研究,招募年满18岁的病理性确诊的肉瘤患者,且要求已有转移、或局部晚期、或不可手术切除,ECOG表现状态0-1分,既往已至少接受过一次系统治疗。患者以非盲的方式分至两个独立的、非对比性的2期试验。按1:1将患者分至纳武单抗组(3mg/kg 2周一次)或纳武单抗联合伊匹单抗组(3mg/kg+1mg/kg 3周一次),各4次剂量。随后,所有患者接受纳武单抗(3mg/kg)单药治疗,2周一次,持续至2年。主要结点:获得可观反应的患者比例。
2015年8月13日-2016年3月17日,在美国的15个点招募了96位患者,其中85位符合要求,43位分至纳武单抗组,42位分至纳武单抗联合伊匹单抗组。纳武单抗组和纳武单抗联合伊匹单抗组获得反应的患者分别有2位(5%[95% CI 1-16]/38)和6位(16%[7-30]/38)。纳武单抗组42位患者中最常见的3级及以上副反应是贫血(4例[10%]),淋巴细胞计数减少(3例[7%]),脱水、脂肪酶增高、疼痛、胸腔积液、呼吸衰竭、次生良性赘生物和尿路梗阻(各2例[5%]);而纳武单抗联合伊匹单抗组42位患者中最常见的3级及以上副反应是贫血(8例[19%])、低血压(4例[10%])、疼痛和尿路感染(各3例[7%])。纳武单抗组和纳武单抗联合伊匹单抗组分别有8例(19%)和11例(26%)严重的治疗相关的副反应,包括贫血、厌食、脱水、血小板计数减少、腹泻、疲劳、发热、肌酐升高、丙氨酸转氨酶升高、天冬氨酸转氨酶升高、低钠血症、疼痛、胸腔积液和瘙痒。无治疗相关的死亡。
鉴于纳武单抗单药治疗肉瘤患者疗效有限,不值得进一步深入研究。纳武单抗联合伊匹单抗,用于特定的肉瘤患者,相比于现采用的治疗方式,疗效可观,且安全性可控。需进行更多的随机研究对纳武单抗联合伊匹单抗的疗效进行深入评估。
原始出处:
Sandra P D'Angelo,et al.Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): two open-label, non-comparative, randomised, phase 2 trials.The Lancet Oncology. January 19, 2018.http://dx.doi.org/10.1016/S1470-2045(18)30006-8
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Lancet#
30
#Oncol#
37
#转移性#
36
是很好的学习材料.不错.以后会多学习.
1
学习了很有用
69
转移性肉瘤患者可选择的治疗方式有限.Nivolumab(纳武单抗)和ipilimumab(伊匹单抗)分别是靶向PD-1和CTLA-4的单克隆抗体.研究人员现对用纳武单抗单独或联合伊匹单抗用于治疗局部晚期.不可手术切除的或转移性肉瘤患者的效果和安全性进行研究.
61
不错的文章值得推荐
66