JAMA:支气管结石——病例报道
2018-07-27 MedSci MedSci原创
患者女性,28岁,因呼吸困难,咳嗽,喘息和咯血(钙化物质的咳出)2周而就诊。患者居住在新英格兰,但之前曾到过内布拉斯加州,科罗拉多州,密西西比州和佛罗里达州。 最近的旅行地点包括乌干达,阿富汗,阿尔巴尼亚和克罗地亚,并经常徒步旅行和露营。无其他病史,不吸烟,不喝酒,不使用非法药物。最初患者接受了吸入沙丁胺醇和口服阿奇霉素治疗,但症状没有改善。 胸部X光片无明显异常。随后的胸部计算机断层扫描(CT)
患者女性,28岁,因呼吸困难,咳嗽,喘息和咯血(钙化物质的咳出)2周而就诊。
患者居住在新英格兰,但之前曾到过内布拉斯加州,科罗拉多州,密西西比州和佛罗里达州。 最近的旅行地点包括乌干达,阿富汗,阿尔巴尼亚和克罗地亚,并经常徒步旅行和露营。无其他病史,不吸烟,不喝酒,不使用非法药物。
最初患者接受了吸入沙丁胺醇和口服阿奇霉素治疗,但症状没有改善。 胸部X光片无明显异常。随后的胸部计算机断层扫描(CT)检查显示,左主干支气管腔内存在结石(图1)。 结核分枝杆菌和真菌及细菌感染检查正常,尿组织浆细胞瘤抗原水平处于临界水平(<0.5 ng/dL)。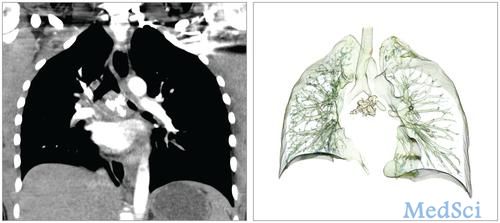
全麻下支气管镜检查显示,近端左主干支气管存在一个6毫米的严重钙化。使用活检钳切除,再通气管。患者术后第二天出院,随访9个月无复发。
原始出处:
de Lima A, Barry M, Majid A. A Young Woman With Cough and Lithoptysis. JAMA. 2018 May 22;319(20):2129-2130. doi: 10.1001/jama.2018.5101.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#支气管#
21
很好的病例,学习了
39
学习了,谢谢分享
35
好文章学习了
42