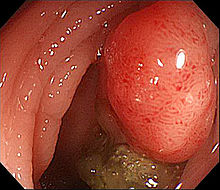
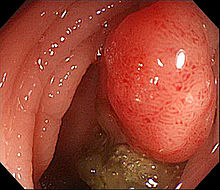
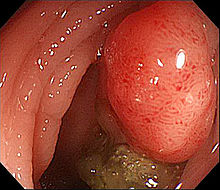
JCO:阿司匹林对结直肠癌患者生存的影响与PD-L1表达有关
2017-04-18 MedSci MedSci原创
阻断PD-1免疫检查点信号通路可以改善肿瘤患者临床结局。有研究证据表明阿司匹林不仅能延长结直肠癌患者生存期,还能激活T细胞介导的抗肿瘤免疫,通过抑制前列腺素E2产生与免疫治疗协同发挥作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
32
#患者生存#
36
#PD-L1表达#
39
学习了,谢谢作者分享!
55
#PD-L1#
36
#结直肠#
23
好有意思!
49