Ann Rheum Dis:引入生物性DMARDs后类风湿性关节炎髋关节和膝关节置换的发生率
2017-12-20 xiangting MedSci原创
在1996年与GPC相比,RA患者中THR和TKR的发生率分别高3倍和14倍。
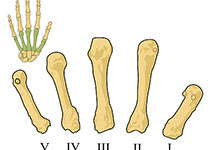
这项研究旨在探讨引入生物性疾病改善抗风湿药物(bDMARDs)和相关类风湿性关节炎(RA)管理指南对丹麦全髋关节(THR)和膝关节置换(TKR)发生率的影响。
这是一项以全国性登记为基础的队列和间断时序分析。在1996年至2011年丹麦全国患者登记中查找偶发性RA患者。RA患者根据年龄、性别和所在市与10个普通人(GPC)相匹配。计算6个月中RA患者和GPC每1000人年THR和TKR的标准化5年发病率。采用分段线性回归,其中间隔1年的滞后期(2002年),对bDMARD前(1996 - 2001年)的水平和趋势与bDMARD时期(2003 - 2016年)进行比较。
共确定了30 404例RA患者和297 916例GPC。1996年,RA患者的THR和TKR发生率分别为8.72和5.87,GPC的发生率分别为2.89和0.42。从1996年到2016年,RA患者THR发病率有所下降,而GPC则有所增加。在RA患者中,TKR的发病率从1996年到2001年有所上升,但从2003年开始下降,并贯穿整个bDMARD时期。1996年至2016年间,GPC的TKR的发病率有所升高。
这项研究发现,在1996年与GPC相比,RA患者中THR和TKR的发生率分别高3倍和14倍。在RA患者中,引入bDMARDs与TKR发病率降低相关,而在bDMARD引入前THR的发生率已经开始下降了。
原始出处:
René Lindholm Cordtz, et al. Incidence of hip and knee replacement in patients with rheumatoid arthritis following the introduction of biological DMARDs: an interrupted time-series analysis using nationwide Danish healthcare registers. Ann Rheum Dis. 15 December 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
23
#RDS#
31
#发生率#
31
#置换#
26
学习谢谢分享!
60
学习一下
77
#关节炎#
28
#类风湿#
32
#DMARDs#
41
#风湿性关节炎#
23